Commentary :
Alan H Rosenstein Healthcare is a complex multidimensional system
that depends upon effective communication and collaboration amongst all members
of the health care team as the key ingredient for best patient care. In the
current health care environment all health care providers are feeling the
growing pressures on care delivery and the changing health dynamics which in
many instances has negatively impacted their attitudes and behaviors toward
medical care. Nursing is a key part of this process. In order to provide best
patient care, affiliated organizations need to recognize how important staff
satisfaction and engagement is to care continuity and provide the necessary
resources and support to maintain staff physical, emotional, and behavioral
well- being. The aim of the article is to review key literature findings to
help organizations recognize the causes and consequences of stress and burnout
and the importance of providing the appropriate support and resources to help
nurses succeed Before
addressing strategies to enhance positive attitudes and behaviors in health
care personnel it is important to recognize the key underlying factors that
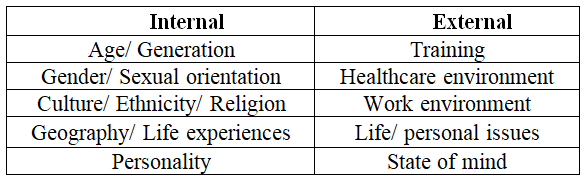
influence an individual’s thoughts and reactions attitudes of individuals are
affected by a number of different factors which I’ll classify as either
Internal or External influencers (Table
1). Table 1: Factors
Affecting Attitudes and Behaviors. The current Coronavirus epidemic has taken an
additional toll as front-line nurses are concerned about access, availability,
safety, and organizational support. More than ever is the importance of
effective teamwork, communication, and collaboration as essential ingredients
to get the job done and prevent any gaps in health care delivery. Many studies
have documented the poor results of dysfunctional care Most of these
inefficiencies are a result of inappropriate human interactions and not system
failure. On the other side, there are many studies that have documented the
positive results of well-coordinated care. These studies demonstrate a direct
correlation between a happy, satisfied, engaged health care team and positive
patient outcomes. Maintaining the well-being of our health care workforce needs
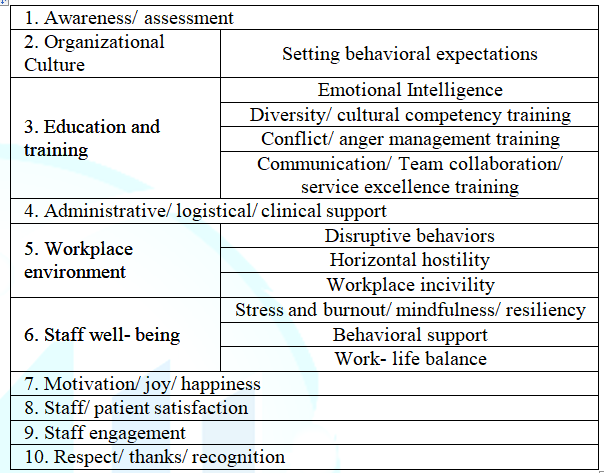
to be a major priority [10-15]. Table 2
lists a number of different strategies for improvement. While the major focus
will be on addressing the importance of attitudes and behaviors of individuals,
it is equally important to address the underlying organizational factors that
impact the healthcare work environment. The first essential is to raise
awareness as to the importance of staff morale and its impact on patient
care. These feelings can be assessed through a number of different survey
tools and/ or by gaining insight through either formal or informal staff input.
Listen, be sensitive, react, and respond to what they have to say. There is a
direct link between staff attitudes and behaviors and organizational culture.
Those organizations that have a strong leadership commitment to staff well-being
and developing a positive work environment do the best in fostering high staff
satisfaction and engagement. As part of this process there needs to be a policy
in place that defines and supports appropriate behaviors with specific criteria
that outlines how non-professional disruptive behaviors will be addressed to
protect staff well-being [16-18]. Health
care is a complex enterprise that requires efficient coordination and
collaboration between all members of the health care team. When healthcare
providers become overextended, overly stressed, or otherwise demoralized, it
can affect attitudes and behaviors that can adversely impact the process and
outcomes of care. Healthcare providers are a precious limited resource and we
need to do everything that we can to help them succeed. We need to listen to
their concerns and provide the appropriate resources to help them adapt to the
pressures of clinical practice. One of the key issues is to keep them happy and
motivated so they can remain engaged. 1. Rosenstein AH. The impact of nurse-physician relationships on nurse satisfaction and retention (2002) American J Nurs 102: 26-34. https://doi.org/10.1097/00000446-200206000-00040 2. Rosenstein AH and Daniel OM. Disruptive behavior and clinical outcomes: perceptions of nurses and physicians (2005) American J Nurs 105: 54-64. https://doi.org/10.1097/00000446-200501000-00025 3. Rosenstein AH and Daniel OM. Negative behavior and clinical outcomes (2005) Nurs Manage 36: 18-28. 4. Rosenstein AH and Daniel OM. A survey of the impact of disruptive behaviors and communication defects on patient safety strategies for creating, sustaining, and improving a Culture of Safety Second Edition Joint Commission Resources 2017 The Joint Commission Oak Brook, IL p.21-28 5. Layne D, Anderson E and Henderson S. Examining the presence and sources of incivility within nursing (2019) J Nurs Management 27: 1505-1511. https://doi.org/10.1111/jonm.12836 6. https://www.beckershospitalreview.com/quality/nurses-work-environments-affect-patient-outcomes-study-finds.html 7. Zhang X and Xiung L. Impact of nurse horizontal violence and coping strategies: a review (2019) Yanktze Med 3: 289-300. https://doi.org/10.4236/ym.2019.34028 8. Backbamis L, Paul D, Smith H and Coustasse A. The burnout syndrome in hospital nurses (2019) Health Care Manage 38: 3-10. https://doi.org/10.1097/HCM.0000000000000243 9. Wan W. Health-care system causing rampant burnout among doctors, nurses (2019) The Washington Post 10. Lai J, Simeng M, Wang Y and Zhongxiang C. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019 (2020) JAMA 3: e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 11. Dang D, Bae SH, Karkwicz K and Kim M. Do clinician disruptive behaviors make an unsafe environment for patients? (2016) J Nurs Care Qual 31: 115-123. https://doi.org/10.1097/NCQ.0000000000000150 12. Layne D, Nemeth L, Mueller M and Martin M. Negative behaviors among healthcare professionals: relationship with patient safety culture (2019) Health Care 7: 23 https://doi.org/10.3390/healthcare7010023 13. https://www.aha.org/news/blog/2017-03-15-focusing-teamwork-and-communication-improve-patient-safety 14. Guck T, Potthoff M, Walters R, Doll J, Michael A, et al. Improved outcomes associated with interprofessional collaborative practice (2019) Annals Fam Med 17: 82. https://doi.org/10.1370/afm.2428 15. Shanafelt T, Gorringe G, Menaker R, Storz K, Reeves D, et al. Impact of organizational leadership on physician burnout and satisfaction (2015) Mayo Clin Proc 90: 432-440. https://doi.org/10.1016/j.mayocp.2015.01.012 16. https://catalyst.nejm.org/organizational-culture-better-health-care/ 17. Rosenstein A. Hospital administration response to physician stress and burnout (2019) Hospital Practice 47: 217-220. http://dx.doi.org/10.1080/21548331.2019.1688596 18. Rosenstein A and Daniel OM. Addressing disruptive nurse- physician behaviors: developing programs and policies to improve relationships that improve outcomes of care (2005) Harvard Health Policy Rev 7: 86-97. 19. Rosenstein A and Stark D. Emotional intelligence: a critical tool to understand and improve behaviors that impact patient care (2015) J Psychol Clin Psyc 2: 1-4 http://dx.doi.org/10.15406/jpcpy.2015.02.00066 20. Rosenstein, A. Addressing physician stress and burnout: impact, implications, and what we need to do (2017) J Psychol Clin Pssyc 7: 1-3. https://doi.org/10.15406/jpcpy.2017.07.00446 21. https://www.nursingcenter.com/getattachment/Clinical-Resources/nursing-pocket-cards/Workplace-Incivility/Workplace-Incivility.pdf.aspx 22. Shanafelt T, West C, Sinsky C, Trockel M, Tutty M, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017 (2019) Mayo Clin Proc 94: 1681-1694. https://doi.org/10.1016/j.mayocp.2018.10.023 23. https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056#3 24. Bakhamis L, Paul D, Smith H and Coustasse A. Still an epidemic: the burnout syndrome in hospital registered nurses (2019) Health Care Manager 38: 3-10. https://doi.org/10.1097/hcm.0000000000000243 25. Shanafelt T, Trockel M, Ripp J, Murphy LM, Sandborg C, et al. Building a program on well-being: key design considerations to meet the unique needs of each organization (2019) Acad Med 94: 156-151. https://doi.org/10.1097/ACM.0000000000002415 26. Dugal L. Re-enchanting medicine (2017) JAMA Intern Med 177: 1075-1076. https://doi.org/10.1001/jamainternmed.2017.2413 27. Linzer L, Sinsky C, Poplau S, Brown R, Williams E, et al. Joy in medical practice: clinician satisfaction in the healthy workplace trial (2017) Health Affairs 36: 1808-1814. https://doi.org/10.1377/hlthaff.2017.0790 28. https://hbr.org/2019/07/making-joy-a-priority-at-work 29. https://nurse.org/articles/nursing-satisfaction-patient-results/ 30. https://americannursetoday.com/physician-nurse-engagement-concept-collaboration/ 31. Sokol-Hessner L, Folcarelli P, Annas C, Brown S, Leonor Fernandez, et al. A roadmap for advancing the practice of respect in healthcare: the results of an interdisciplinary modified delphi consensus survey (2018) The Joint Commission J Quality Safety 44: 463-476. https://doi.org/10.1016/j.jcjq.2018.02.003 32. https://hbr.org/2020/05/in-times-of-crisis-a-little-thanks-goes-a-long-way Alan H
Rosenstein, Practicing Internist and Consultant in Physician Behavioral
Management, San Francisco, California, USA, +Tel: 415 370 7754, E-mail: ahrosensteinmd@aol.com Rosenstein
HA. The impact of attitudes and behaviors on nurse satisfaction, well-being,
and outcomes of patient care (2020) Nursing and Health Care 5: 15-17. Patient care, Nursing, BehaviorThe Impact of Attitudes and Behaviors on Nurse Satisfaction, Well-being, and Outcomes of Patient Care
Abstract
Full-Text
Background
Factors Affecting
Attitudes and Behaviors
Recommendations
References
*Corresponding author
Citation
Keywords