Research Article :
Ideal
health is the ultimate goal of mankind throughout all ages. As the age advanced
several medical problems and diseases occurs, which have an underlying cause as
nutritional aspects and along with that patients socioeconomic status and his
dietary habits have a profound influence on their dietary selection. Ideal
health is the ultimate goal of mankind throughout all ages. Proper nutrition
contributes in expression of proper genetic heritage. Consequently, severity of
age related degenerative
disease might be influenced by nutrition. As
the age advances several medical problems and diseases occurs, which have an
underlying cause as nutritional aspects and along with that patients
socioeconomic status and the dietary habits have a profound influence on their
dietary selection [1]. Hence,
a dental
professional must also be aware of these potential
detrimental effects of dental treatment and provide counteractive dietary
guidance. The aim of this review is to summarize the earlier investigations on
the association between food intake and dental
status in geriatric patients [2]. Oral
health is a prerequisite for a good chewing
function, which may have an impact on food choice and nutritional well-being
[3]. A variety of oral conditions can lead to an inadequate nutritional status,
including tooth loss, pain and discomfort associated with caries, periodontal
disease and ill-fitted dentures [4]. The
absence of teeth in particular can affect the digestive capacity and
nutritional status of the individual. Furthermore, the selection of food can be
impaired due to the reduced masticatory capacity of the individual, leading to
a restricted intake of fiber and protein-containing foods [5]. The presence of
natural teeth and well-fit dentures has been linked to an increased variety of
foods and nutrient intake, which will contribute to the consumption of a diet
rich in fiber [6]. Maintaining an adequate nutritional status is important
because an inadequate health status can lead to either underweight, which
increases the risk of infections and mortality [7]. Healthy
teeth are essential for effective chewing and
swallowing and therefore for good nutrition intake. The relationship
between oral health and nutritional health in the
elderly is complex and controversial, and current understanding of it is
limited [8]. Nutritional status also acts as a determination factor for
physical performance with aging [9,10]. Nutritional status has been reported to
deteriorate with aging, partly due to the loss of muscle mass and declined food
intake [11]. Food avoidance and food modification are two self-management
strategies [12]. Those who have impaired oral health may avoid foods that are
difficult to eat or modify the ways that foods are prepared or eaten. Each can
serve a different purpose. Without regard for the impact on the nutritional
quality of the diet, avoidance can minimize the effects of chewing difficulties
and tooth pain, and other oral health problems [13]. Modifying foods may serve
to maintain certain foods in the diet that one perceives as beneficial or
pleasant, and overcome difficulties with the inability to chew food properly
[16]. The
aim of this study is to evaluate the relationship between oral health status
and nutritional status of non-institutionalized elderly individuals. The effect
of aging on the oral health status, the effect of the oral health status on
nutritional intake and the correlation of oral
health status and malnutrition in the elderly will be
evaluated. We hypothesize that there is a correlation between the oral status
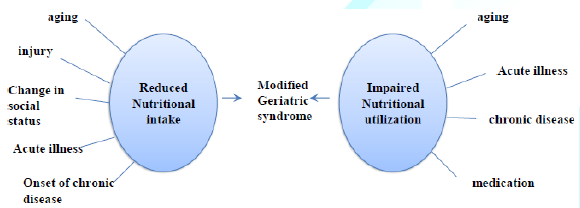
and the nutritional intake in elderly people (Figure 1). Figure 1:
A frame work of the review of literature. This
is a Cross sectional research of geriatric outpatients who visited RAKCODS
Dental Clinic. The duration of this research was six months. The study plan had
been approved by the Ethics Committee of the University (RAK.REC.REF
24-2016-UG). Patients Groups:
40 geriatric patients (20 males and 20 females) were participated in this
research. All the participants were signed on Consent form (Questionnaire Provided as Supplementary).
For illiterate or low-reading level subjects, consent was obtained through
their legal representatives. Excluded from the study were those individuals
that were not in good enough physical and/or mental condition to participate in
the collection of data, for example: those confined to wheelchairs, amputees,
or those with problems of understanding that would prevent the measurements
used in the study from being taken. The sample was divided into two groups, the
Young Senior Group (YSG), with age not exceeding 70 years, and the Elderly
Senior Group (ESG), aged over 70 years. The
cut-off point for the definition of elderly recommended by the World Health
Organization (WHO) (1989). The
Data collecting procedure will be in the following process: · History
taking, · Questionnaires,
to collect information on socioeconomic status, eating habits, physical
activity and health habits, · Clinical
examination and radiographic analysis. The oral health status was assessed
using the index for Decayed,
Missing and Filled Teeth (DMFT). The evaluation of oral
health status included the identification of decayed, missing, and filled
teeth, and the presence of prostheses. The oral examination was conducted in
daylight according to biosecurity standards and the findings reported in an
odontogram as recommended by the WHO (1997). The
data were analyzed using chi test statistics to assess the different factors
affecting the oral status of the participated groups. For comparison and
analysis of results the cut-off values used were those obtained from the Oral
Health Survey of 2003 for the elderly age group (65 to
74 years) carried out in the Southeast region of Brazil. The mean DMFT for this
region was 28.61 ± 6.44 which meant that dental health was satisfactory, this
being defined when DMFT ≤ 22.17, with dental health status considered poor when
DMFT>22.17. By transforming the DMFT index in Decayed (D), Missing (M) and
Filled (F) the cut-off point was the average found in the Southeast where oral
health status had satisfactory values of D>0.60, M>27.05 and F=0.91, and
oral health status was poor with D>0.60, M>27.05 and F>0.91. The
Kappa test was used to lend a greater reliability to the data collected, and
the value of k was =0.9129, with a p-value below 0.01%. The importance of this
test is that it shows that the value of K was significantly different from zero
and this association is classified as excellent. Other data on the oral health
status were obtained with direct questions about intake of types of food and
perception of the quality of dental prostheses. The
data obtained were presented in descriptive form as mean, standard deviation
and percentage. For comparison of continuous variables between the two groups,
we used Students t-test for independent samples or the Mann-Whitney test. To
examine the correlations between continuous variables we used Pearsons
correlation test or Spearmans. For the correlations between variables, we used
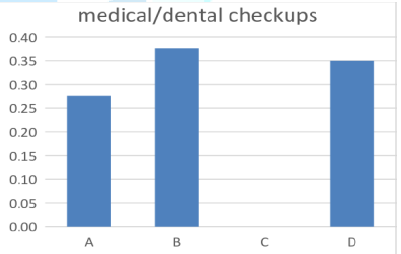
Fischers exact test. Figure
2: Results according to the medical and dental
checkups. The
question was Do you maintain regular visits with your physician and dentist? A.
Yes, I maintain regular visits with my physician and dentist. B.
No, I only maintain regular visit with my physician. C.
No, I only maintain regular visit with my dentist. D.
No, I dont maintain regular visit with either. 70%
from the patients have chooses answer B (0.38%) and D (0.35%) but the
significance is in answer C to not able to maintain regular visits with the
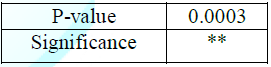
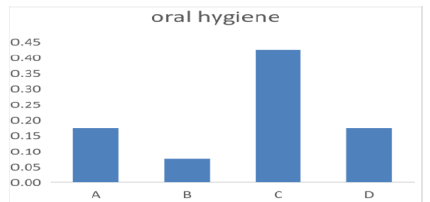
dentist (0.50%). So, P-value was C significant answers (0.0003) (Figure 2 and Table 1). Figure 3:
Results according to oral hygiene. The
question was Do you brush and floss your teeth or use mouth wash? A.
Yes, I brush and floss daily and use mouth wash. B.
Yes, I brush my teeth and floss but i dont use mouthwash. C.
Yes, I only brush my teeth but not daily. D.
No, I dont do anything to my teeth. Majority
answered C (0.47%), and according to the oral hygiene scale majority had fair
scale (P-Value 0.0008) (Figure 3 and Table
2). They
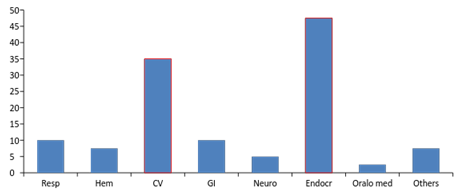
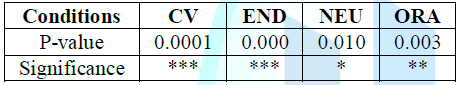
increase in prevalence of cardiovascular
disease and endocrine
disease, out of 40 samples 19% had endocrine
and 14% had cardiovascular conditions. There is a minor significant in
neurological disease and its prevalence in geriatric population, only 2% of the
population had neurologic conditions (Figure
4 and Table 3). Figure 4: Results
according to systemic disease. Table 3:
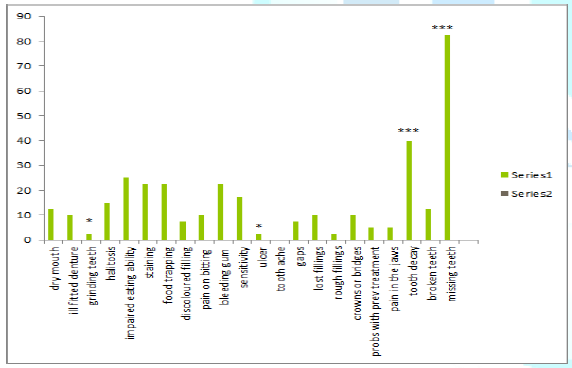
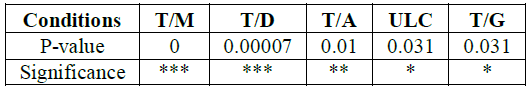
P-value of the significances according to the systemic disease. Majority
of samples had missing teeth and tooth decay regardless of gender, while none
of the samples had any tooth aches which showed a significance, and minor
significance in patients with grinding
teeth habit and
tooth ulcer (Figure
5 and Table 4). Figure 5:
Results according to oral diseases. Table 4:
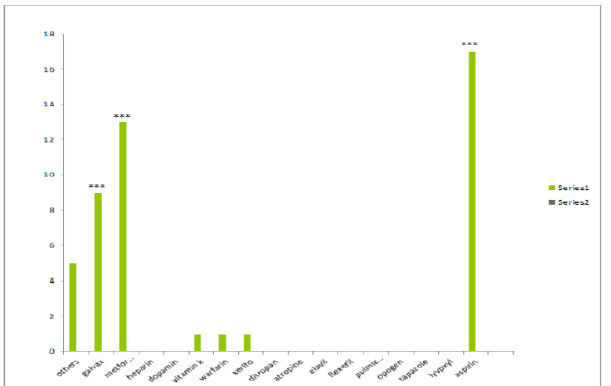
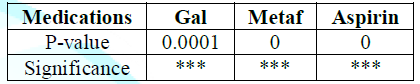
P-value of the significances according to the oral conditions. There
is increase in prevalence and significance with patients taking galvax and
metformin and aspirin in the geriatric
population (Figure
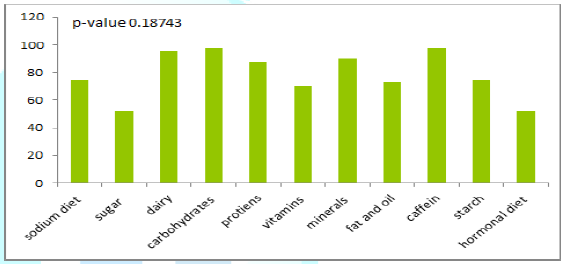
6 and Table 5). According
to the graph (no significance has been found) (Figure 7). 97.5% of the geriatric sample includes carbohydrates
and caffeine and dairy and protein in their diet, nevertheless 52% include
sugar and 75% include sodium in their diet, which reveals change in diet
according to the systemic diseases. Figure 6:
Results according to the choice of medications. Table 5:
P-value of significance according to the medications. Figure 7:
Results according to diet selection. The
purpose of this study is to determine if there are associations between
nutritional intake and the oral health status in geriatric population. There is
an abundant scientific evidence to support the involvement of oral
health in general health. Some authors have described the
role of oral health is in nutrition, and indirectly in the control of different
acute and chronic diseases. In the present study, we found that changes in diet
can influence the oral health and vice versa. Reflecting in the nutritional
status of the individual Review of the study has shown that patients who have
marked loss of teeth may be prone to a decrease in the intake of foods with a
heavy consistency, which are a major source of vitamins, minerals, fiber and
protein. However, it is important to note that there are several factors other
than oral health status that influence food choice, such as personal
preferences, available food sources and dietary habits, as well as psychosocial
and economic factors [2]. From
a theoretical viewpoint, given that oral health is a modifiable risk factor,
its improvement would reduce the risk of mastication and swallowing problems
and the nutritional deficiencies they can cause. Deficient mastication is
related to tooth loss, a lack of saliva, mastication force, and malocclusion
problems. Some local studies have indicated that individuals with mastication
problems avoid fresh fruits and vegetables, well-done meat, and even bread, preferring
soft, easily chewable food that can often raise sugar and fat consumption to
levels above recommendations, increasing their risk of cardiovascular diseases
and metabolic syndrome. Masticatory function in elderly depends on two major
factors, which are the number of natural antagonist teeth and the quantity and
quality of saliva. Subsequent potential nutritional consequences are generally
considered according to two different viewpoints. The first viewpoint considers
a healthy oral aging taking place without any important oral
disorders such as tooth loss or critical
saliva deficiency. For this segment of population,
aging is associated with a decrease in maximal bite force and changes in
Masticatory muscle tissue. However, these alterations have little impact on
Masticatory performance as these persons still produce a food bolus suitable
for swallowing and only minor adaptations are needed to compensate the
physiological changes. The
second viewpoint considers the impact of oral functioning on digestion or
nutritional status in the elderly. In addition, denture wearers fail to adapt
to changes in food texture such as hardness. A recent review of the evidence
for nutritional exposures in the etiology of periodontitis suggests that, in
some cases, inadequate levels of vitamin D and calcium may contribute to
periodontal disease and that nutritional intervention may be of some benefit
[15]. According to this survey it has shown that majority add dairy and protein
in their diet which showed uncommon periodontal disease in the sample taken. In
a recent study, severe tooth loss in older adults was found to be a key
indicator of a compromised dietary quality [16]. And an impaired oral health
often leads elderly to modify their diet to adjust it to their limited oral
functional capacities. These changes are mostly not adequate to maintain good
overall health since soft foods are often foods rich in fat and contain
additives [17]. In
summary, the oral health status of the geriatric population is generally
deficient, with an elevated prevalence
of caries, periodontal disease, and tooth loss.
These are responsible for mastication difficulties, chronic disease
destabilization, and impairment of oral quality of life, with direct effects on
the individuals general quality of life and well-being. Surveillance and
improvement of the oral health of the elderly should be a key objective of the
multidisciplinary team responsible for their care, including dentists, dental
hygienists, geriatricians, and caregivers. According
to the systemic disease patients regardless of age group and gender showed that
majority had cardiovascular and endocrine diseases which lead them to use
medications such as galvex and metformin and aspirin and eventually change
their diet accordingly, by reducing their sugar and sodium intake. The major
significant oral conditions in this study were missing teeth and decayed teeth
while minor significance showed in tooth
ache and ulcer in the geriatric population. Increase
carbohydrate intake nevertheless decrease in sugar and sodium intake in their
diet specifically showed unhealthy diet selection in regards of their
limitation in diet selection, which as mentioned earlier choice of diet
preference may be because of several factors such as socio economic status and
educational factors. According to the number of elderly participants in this
pilot study, it may be concluded that the DMFT index was satisfactory in 60.7%
of the patients. Tooth loss was the biggest concern of the elderly in
accordance with the high percentage of ill-fitting dentures (45.5%) and
prostheses that make it difficult to chew (51.5%). The
main recommendation is to modify the consistency of the diet, eliminating
certain foods and reducing the possibility of nutritional defects. Balanced
diet as nutritional recommendations for Oral
Healthcare team as the general assessment that tooth loss
in elderly people who need nursing care is likely to have a larger impact on
nutrition than that in healthy elderly people 1.
Gil-Montoya JA, Ferreira de Mello
AL, Barrios R, Gonzalez-Moles MA and Bravo M. Oral health in the elderly
patient and its impact on general well-being: a nonsystematic review (2015)
Clin Interv Aging 10: 461-467. https://doi.org/10.2147/cia.s54630
2.
Rodrigues Junior HL, Scelza MFZ, Boaventura
GT, Custódio SM, Moreira EAM, et al. Relation between oral health and nutritional
condition in the elderly (2012) J Appl Oral Sci 20: 38-44. https://doi.org/10.1590/s1678-77572012000100008
3.
Rauen MS, Moreira EA, Calvo MC
and Lobo AS. Oral condition and its relationship to nutritional status in the
institutionalized elderly population (2006) J Am Diet Assoc 106: 1112-1114. https://doi.org/10.1016/j.jada.2006.04.015
4.
Touger-Decker R and Mobley CC. Position
of the American Dietetic Association: oral health and nutrition (2007) J Am Diet
Assoc 107: 1418-1428. https://doi.org/10.1016/j.jada.2007.06.003
5.
Sheiham A and Steele J. Does the
condition of the mouth and teeth affect the ability to eat certain foods,
nutrient and dietary intake and nutritional status amongst older people (2001)
Public Health Nutr 4: 797-803. https://doi.org/10.1079/phn2000116
6.
Marshall TA, Warren JJ, Hand JS, Xie
XJ and Stumbo PJ. Oral health, nutrient intake and dietary quality in the very
old (2002) J Am Dent Assoc 133: 1369-1379. https://doi.org/10.14219/jada.archive.2002.0052
7.
World
Health Organisation (1995) Tech Rep Ser 854:1-452. 8.
Muirhead VE, Marcenes W and Wright
D. Do health provider-patient relationships matter? Exploring dentist-patient
relationships and oral health-related quality of life in older people (2014)
Age Ageing 43: 399-405. https://doi.org/10.1093/ageing/aft183
9.
Alipanah N, Varadhan R, Sun K,
Ferrucci L, Fried LP, et al. Low serum carotenoids are associated with a
decline in walking speed in older women (2009) J Nutr Health Aging 13: 170-175.
https://doi.org/10.1007/s12603-009-0053-6
10.
Houston DK, Stevens J, Cai J and
Haines PS. Dairy, fruit, and vegetable intakes and functional limitations and
disability in a biracial cohort: the Atherosclerosis Risk in Communities Study
(2005) Am J Clin Nutr 81: 515-522. https://doi.org/10.1093/ajcn.81.2.515
11.
Volkert D. Malnutrition in the
elderly-prevalence, causes, and corrective strategies (2002) Clin Nutr 21: 110-112.
https://doi.org/10.1016/s0261-5614(02)80014-0
12.
Quandt SA, Chen H, Bell RA,
Savoca MR, Anderson AM, et al. Food avoidance and food modification practices
of older rural adults: association with oral health status and implications for
service provision (2010) Gerontologist 50: 100-111. 13.
Chavers LS, Gilbert GH and
Shelton BJ. Two-year incidence of oral disadvantage, a measure of oral
health-related quality of life (2003) Community Dent Oral Epidemiol 31: 21-29.
https://doi.org/10.1034/j.1600-0528.2003.00031.x
14.
Anastassiadou V and Heath MR. Food
choices and eating difficulty among elderly edentate patients in Greece (2002)
Gerodontology 19: 17-24. https://doi.org/10.1111/j.1741-2358.2002.00017.x
15.
Van der Velden U, Kuzmanova D and
Chapple ILC. Micro nutritional approaches to periodontal therapy (2011) J Clin
Periodontal 38: 142-158. https://doi.org/10.1111/j.1600-051x.2010.01663.x
16.
Savoca MR, Arcury TA, Leng X,
Chen H, Bell RA, et al. Severe tooth loss in older adults as a key indicator of
compromised dietary quality (2010) Public Health Nutr 13: 466-474. https://doi.org/10.1017/s1368980009991236
17.
Rémond D, Shahar DR, Gille D,
Paula P, Kachal J, et al. Understanding the gastrointestinal tract of the
elderly to develop dietary solutions that prevent malnutrition (2015)
Oncotarget 6: 13858-13898. https://doi.org/10.18632/oncotarget.4030
Hala Zakaria, Associate
Professor, RAK College of Dental Sciences, RAK Medical and Health Sciences
University, United Arab Emirates, E-mail: hala.zakaria@rakmhsu.ac.ae Zakaria H,
Duarte C, Falah H and Abdulwahab M. Assessment of correlation between nutrition
and oral status of elderly (2020) Dental Res Manag 4: 4-7. Diet, Geriatrics, Nutritional analysis, Dental
status may influence food intake.Assessment-of-Correlation-between-Nutrition-and--Oral-Status-of-Elderly
Hala Zakaria,
Carolina Duarte, Hadeel Falah and Maryam Abdulwahab
Abstract
Aim: This research is to summarize the earlier
investigations on the association between food intake and dental status in
geriatric patients.
Study Design: Cross sectional Study by clinical Data Collection.
Place and Duration of Study: Six months in RAK College of Dental Sciences
outpatient Clinic.
Methodology: The information analysis was taken from geriatric
patients from RAK outpatient clinic. The sampling methods of the patients are
categorized by the gender, and health status, and habits for each gender. The
numbers of the patients are approximately 40 patients, 20 male, and 20 female.
The patients from both genders are also categorized based on habits, and health
issues. A set of questions will be presented as a questionnaire paper to the
patients.
Results: The results of data collection have shown that the
patients regardless of age group and gender showed that majority had
cardiovascular and endocrine diseases which lead them to use medications such
as galvex, metformin and aspirin which also they eventually changed their diet
accordingly, by reducing their sugar and sodium intake. The major significant
oral conditions in this study were missing teeth and decayed teeth while minor
significance. The major significant oral conditions in this study were missing
teeth and decayed teeth while minor significance showed in tooth ache and ulcer
in the geriatric population. Increase carbohydrate intake nevertheless decrease
in sugar and sodium intake in their diet specifically showed unhealthy diet
selection in regards of their limitation in diet selection, which as mentioned
earlier choice of diet preference may be because of several factors such as
socio economic status and educational factors.
Conclusion:
The changes in diet of geriatric individuals can strongly influence on the oral
health. The oral health status of the geriatric population is generally
deficient, with an elevated prevalence of caries, periodontal disease and tooth
loss. Hence, a dental professional must be aware of these potential detrimental
effects of dental treatment and provide counteractive dietary guidance. Full-Text
Introduction
Review of the Literature
Materials and Method
Results

Discussion
Conclusions
Recommendations
References
*Corresponding author
Citation
Keywords