Case Report :
Hugo Romero, Charlotte Medina Montoya, Hernan Enrique Yanes Moya and VilmaUmanzor Gorlin-Goltz Syndrome (GGS) also known as Nevoid
Basal Cell Carcinoma Syndrome is a rare autosomal dominant disorder. Is
characterized for presenting some clinical features such as palmar pits, fused
eyebrows, multiple odontogenic keratocyst, which are considered some of the
most common signs. In our case, a rare familial case highlights awareness when
a member of the family is diagnosed with this condition, and the probability to
find in one the first degree relative. Once again it is confirmed that is
impossible to determine without the radiographical analysis such as Cone Beam
Computed Tomography (CBCT), ortophantomography, magnetic resonance imaging, to
corroborate with clinical aspects, advising that, this could be the best way
for the sake of patients benefit. Many treatments less aggressive have been
proposed along the years, with a lower percentage of success against the
traditional way, specifically surgical enucleation/marsupialization combined
with peripheral osteotomy, in order to approach the variable behavior of nevoid
basal cell carcinoma syndrome. The early diagnosis is considered the key to
well manage this kind of disease, due to its aggressiveness, potential to
become malignant, and in some cases, with a silent destructive pattern. Gorlin-Goltz
syndrome also known as Nevoid
Basal Cell Carcinoma Syndrome was described for the first time in 1894 from
Jarisch and White [1]. Later in 1939, Straith described a familiar case in
which multiple basocellular carcinomas and cysts appeared. In 1953, Gross
presented a case suggesting additional signs such as synostosis of the first
left rib and bilateral bifurcation of the sixth ribs. On the other hand,
Bettley and Ward were the first to relate the presence of palmar and plantar
pits with this syndrome. Nevertheless, it was not until 1960 when Robert James
Gorlin and William Goltz established classical triad that characterizes the
diagnosis of this syndrome (multiple basocellular epitheliomas, keratocysts in
the jaws and bifid ribs [2]. Later this triad was modified by Rayner et al.,
who established that cysts had to appear simultaneously, either with
calcifications of the falx cerebri, or with palmar and plantar pits, in order
to arrive at a diagnosis [3]. The porpoise is discussing one familial case of
Gorlin Goltz Syndrome and describing the characteristics and features this
syndrome expresses. A
patient of 18-year-old was referred to our hospital with a chief complaint of
pain in the mandible accompanied with swelling in bilateral retromolar zone and
symphysis area. Patient presented sensibility and mobility in lower dental
pieces. Physical examination revealed fused eyebrows, mandibular prognatism,
mild hypertelorism, bony bridging of sella turca, odontogenic
keratocysts, punctat dyskeratotic pits on hand and face (Figure 1 and Figure 2), and
hyperneumanization of paranasal sinuses. Figure 1: Frontal profile of the patient. The
CBCT (Figure 3) and the orthopantomogram
(Figure 4) was advised which
revealed three cystic
lesions in mandibular bone, one in the symphysis and one on each side of
the mandibular angle, and two involving the maxillary canine region on both
sides with the displaced permanent teeths. It also revealed dental agenesis of
1.8, 2.6, 2.7, 2.8, 3.8 and 4.8. The 1.3, 2.3, 3.3, and 3.7 were displaced owed
to the presence of keratocysts. The odontogenic keratocyst typically shows a
thin, friable wall, which if often difficult to enucleate from the bone in one
piece. The cystic lumen may contain a clear liquid that is like a transudate of
serum, on microscopic examination consists of keratinaceous debris. Figure 3: Cone beam computed tomography. Multiple
odontogenic keratocysts are seen in 85% of cases, nearly all of which
develop between the ages of 7 and 40 years. The peak age of development is
between 12 and 25 years. Odontogenic keratocysts develop three times more
frequently in the mandible than in the maxilla. The growth rate and
aggressiveness of odontogenic keratocysts associated with basal cell nevus
syndrome are no different than those associated with isolated odontogenic
keratocysts. However, the emergence of odontogenic keratocysts from odontogenic
[4]. Microscopically,
the thin fibrous wall is essentially devoid of any inflammatory infiltrate. The
epithelial lining is composed of a uniform layer of stratified squamous
epithelium, usually six to eight cells in thickness. The epithelium and
connective tissue interface is usually flat, and rete ridge formation it’s inconspicuous
(Figure 5) [5]. The
patient was asked about the other family members and revealed that his mother,
sister, and brother had similar characteristic lesions. His mother was
diagnosed at the age of 27, her principal complain was pain in the lower jaw,
specifically in the mental zone (Figure
6). The orthopantomogram showed four dark radiolucent lesions compatible
with odontogenic keratocyst. Biopsy was performed to confirm the disease (Figure 7). Figure 6: Frontal profile of the mother. The
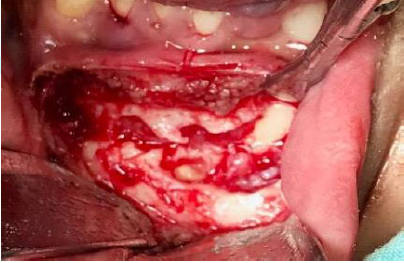
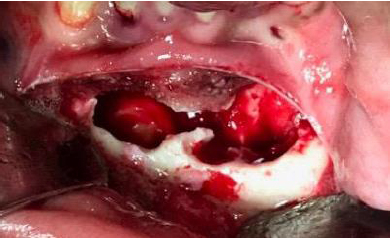
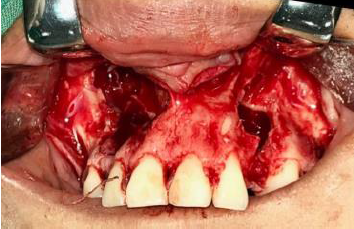
patients underwent surgical treatment for elimination of the jaw
and maxillary cysts with general anesthetic. At first, we approached the
maxillary with a periodontium flap discovering the cysts, we continued with an
enucleation with peripheral osteotomy of left cyst involving the upper left
canine and then with the enucleation with peripheral
osteotomy of the right cyst involving the upper right canine repositioning
the periodontium flap afterwards. Then we proceed with the lower jaw starting
with a periodontium flap of the left cyst located in the body of the jaw, the
symphysis cyst and the right angle of the jaw cyst perferming an enucleation
with peripheral osteotomy finishing with the repositioning of the periodontium
flap. The monetary capability of the patient and the lack of supplies of
the hospital made it impossible to use any bone substitute nonetheless the
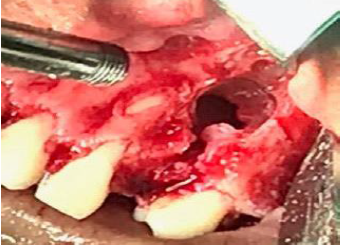
result of the surgery was good (Figure 8
to Figure 15). Figure 8:Odontogenic Keratocyst, symphysis area. Figure 9: Removed odontogenic keratocyte in symphysis area. Figure 10: Odontogenic Keratocyst surrounding upper right canine. Figure 11: Exposing Odontogenic Keratocyst. Figure 12: Odontogenic Keratocyst surrounding upper left canine. Figure 13: Removed odontogenic keratocyst surrounding the left canine. Figure 14: Removed left and right odontogenic keratocysts Figure 15: Retromolar zone cavity. Patient
was followed up four months, where he presented bone regeneration, stability of
dental pieces, no paresthesia, and lack of swelling and better breath smell (Figure 16). Figure 16: Four Months followed up panoramic radiography Do
to the genetical component and aggressive
behavior of Gorlin Goltz Syndrome, the decision to advise a control
orthopantogram for his sister, revealed one cyst in left base of the mandible (Figure 17). Odontogenic
Keratocyst is considered by the WHO as a benign and multicystic, intraosseous
tumor of odontogenic origin with a characteristic location of parakeratinized
squamous epithelium with defined as a potentially aggressive, infiltrating
behavior [6]. In differential diagnoses are to be mentioned: • Follicular
cyst • Ameloblastoma • Ameloblastic
fibroma • Odontogenic
Myxofribroma • Plasmocytoma
(multiple myeloma) • Aneurysmal
bone cyst To
confirm the diagnosis of odontogenic keratocyst, a histological examination as
a trial biopsy or examination of the entire primary removed cyst bladder [6]. The
Gorlin-Goltz syndrome is an autosomal dominant inherited syndrome manifested by
multiple defects involving the skin, nervous system, eyes, endocrine system,
and bones. It is also known as basal cell nevus syndrome, multiple basal cell
carcinoma syndrome, Gorlin syndrome, or hereditary cutaneomandibular
polyonocosis, multiple nevoid basal cell epithelioma-jaw cysts, or bifid rib
syndrome [7]. The
incidence of this syndrome is estimated to be 1 in 50,000 to 150,000in the
general population bur perceived incidence may vary by region. There is no
racial/ sex predilection associated with Gorlin syndrome [8]. The
tumor suppressor gene called Patched (PTCH), located in the 9q22.3 chromosome,
has been identified as the cause of Gorlin-Goltz syndrome. Data suggest that a
product of this gene acts as tumor suppressor and Gorlin- Goltz syndrome’s
typical malformative patterns suggest that the main function is to control the
growth and development of normal tissues [1,9]. The
diagnostic criteria for nevoid basal cell carcinoma was established by Evans et
al., and modified by Kimonis et al. in 1973. According to them diagnosis of
Gorlin-Goltz syndrome can be established when two major or one major and two
minors are present which are described below [7]. In
our patient showed three major criteria’s, three odontogenic keratocyst in jaw
and two in maxilla, palmar pits and a first degree relative. Minor criteria
were such as fused eyebrows, prognathism, hyperpneumanization
of paranasal sinuses and bony bridging of sella turca. In the mandible, 43%
Odontogenic keratocysts (OKCs) occurs in the molar ramus region, followed by
18% in the incisor-canine area. In the maxilla, 14% OKCs were found to occur in
the incisor-canine area, followed by molar tuberosity with 12%, 7% in the
mandibular premolar region and 3% in the maxillary premolar region [11]. There
are two methods of treating odontogenic keratocysts: Conservative or
aggressive. In the conservative method, simple enucleation with or without
curettage and marsupialization are suggested. Aggressive methods include
peripheral ostectomy, chemical curettage with Carnoy's solution and resection
[3]. Cryosurgery
using liquid nitrogen is indicated in the large complex mandibular
lesions if there is a risk of damage to vital structures with conventional
treatment methods [10]. The liquid nitrogen treatment showed very good results
[1].
Gorlin
Goltz syndrome is an autosomal dominant mode of inheritance, in this case from
the mother to her children. Major and minor criteria must be present when
identifying odontogenic keratocyst for diagnoses this syndrome. Radiographic
and genealogical analysis is essential to establish an accurate and early
diagnosis. Hugo Romero, Professor and Head Department of Oral
and Maxillofacial Surgery, National Autonomous University of Honduras (UNAH), Private
practice, Tegucigalpa, Honduras, E-mail: cmfalvarenga@gmail.com
Romero H, Montoya CM, Moya HEY and
Umanzor V. Gorlin-goltz syndrome: A familial case report (2020) Dental Res
Manag 4: 42-45. Gorlin goltz syndrome, Odontogenic keratocyst,
Palmar pits, Nevoid basal cell carcinoma syndrome.Gorlin-Goltz Syndrome: A Familial Case Report
Abstract
Full-Text
Introduction
Case Report
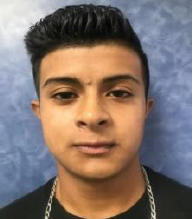



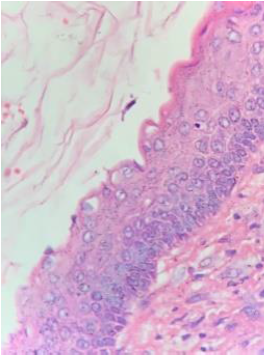
Figure 5: OdontogenicKeratocyst: The epithelial lining is from 6 to 8 thick.







Discussion
Treatment
Conclusion
References
Citation
Keywords