Human deaths due to cancer have risen sharply, in recent years. Cancer is one of the most important causes of morbidity and mortality, worldwide, with nearly 14 million new cases in 2012 [1]. It, also, remains the second leading cause of death in the world and is responsible for 8.8 million deaths in 2015 [2]. In Greece, cancer is the second leading cause of death and accounts for about 25,000 deaths a year, according to the latest measurements [3]. Diagnosis of cancer is likely to cause uncertainty and anxiety to patients, emotions that can be eliminated by providing timely and valid information regarding diagnosis, prognosis and treatment options.
Patients’ awareness of cancer diagnosis and integrated communication with healthcare professionals are found to be essential for the effective management of the disease, as well as, the reduction of emotional transitions, improved patients’ quality of life and communication with family members [4-8]. Although, studies from different countries support the fact that the majority of patients with cancer need to be well informed about diagnosis and cancer treatment and more active in the decision-making process, there are still many cancer patients unaware of their true diagnosis, worldwide, an attitude that is considered acceptable in many societies [9-14]. Particular emphasis has also been given in recent decades on patients’ autonomy and their involvement in decisions regarding treatment [15-16].
Patients’ roles in treatment decision making can differ from playing a passive role, where all decision are made by the physician, through sharing role, to an active role, in which patients decide themselves about treatment. In the United States, National health organizations Recommend the inclusion of patients in decision-making procedures [8,17]. However, researches support that patient’s wish to more information and participation in decision making is personalized, may change through time and can be influenced by social, economic and cultural factors, while other studies result that patients wishes are often underestimated by healthcare professional for various reasons [2,5,16,18-21].
The latest international literature review shows that cancer patients are more active than ever in the decision-making process. Specifically, 75% of cancer patients with hematological malignancies chose the shared decision-making according to a recent study in Netherlands. Also, in a study in USA the majority (53%) of the 119 Hispanic American patients preferred shared decision-making with their doctor, while only 7,6% had a passive decision-making style [22,23].
In Greece, paternalism is not challenged yet and the consumerist model of health care is not strongly developed [6]. In recent years, choices of cancer treatment are discussed with some patients, depending on factors such as educational level, age and health status, however, Greek physicians often decide on their own the most appropriate treatment, without having informed the patient first about the disease and the available treatment options. In 2005, Greek general practitioners reported that heavy workloads and lack of time are responsible for incomplete information and promotion of counseling to cancer patients [24].
Consequently, the aim of this study was to evaluate Greek cancer patients’ awareness of diagnosis, nowadays, and assess their decision-making preferences regarding treatment. Very few studies have been conducted in Greece regarding awareness of cancer diagnosis, with the majority of them being conducted in the previous decade and only two studies have been carried out regarding decision-making preferences among Greek cancer patients [6,16,25-27].
Methods
Study
Design and Participants
It
was a cross-sectional study, conducted in a large general public hospital of Athens.
316 cancer patients were collectively treated in the pathology
clinics and the outpatient department of the study hospital, from January 2013
to August 2014. The inclusion criteria used were
- Histologically
documented diagnosis of cancer,
- 18
or more years of age,
- Verbal
communication ability and fluency in spoken and written Greek language
- Consent to participate in the study.
The
exclusion criteria used were
- Alcohol
and/or drug abuse,
- Dementia,
- Brain
metastasis,
- History
of psychotic illness,
- Existence
of other life threatening disease
- Ignorance
of diagnosis.
The first five exclusion criteria were used because their existence could affect patients’ consciousness and perception during the interview but also their answers regarding their preferences on their role in treatment decisions of the 316 patients, 21 had an individual history of psychiatric disease, 46 patients had Alzheimer's disease or a form of dementia and 13 patients had a co-existing life-threatening disease (5 patients had end-stage heart failure and 8 patients had chronic renal failure under hemodialysis).
According
to the inclusion criteria, 236 patients could have been admitted to the study.
Out of those patients, 229 agreed to participate in the study (response rate
97.03%). The sixth exclusion criterion was used subsequently for the admission
at the Control Preference Scale tool. The final sample of patients that
completed the CPS-Greek edition questionnaire was 209.
Collection
of Data and Measures
Demographic data, diagnosis and clinical characteristics were obtained by patients’ medical records review. Adequate data were collected by means of semi structured interviews. The Control Preference Scale (CPS) instrument was used in this study for the assessment of patients’ decision-making preferences. Patients were evaluated as to whether they had knowledge of their diagnosis and what this was through interview. Those who knew their diagnosis was cancer (n=209) were administered to the CPS tool.
The CPS created by Degner et al. [28] is an assessment tool which measures the decision-making preferences of cancer patients [29]. It is a clinically relevant, easy-to-administer, reliable and valid measure of roles (preferred and actual) in decision making on health care issues among cancer patients [30]. It consists of five cards (A to E), each describing a potential role of the patient in relation to the physician, whenever a decision about treatment is made. Every card has a statement that describes the role and is illustrated by a cartoon in order to assist patients of lower literacy level to understand the meaning. The roles range from (A) the patient being the primary decision maker, (C) shared decision making, to (E) patient being completely passive to the physician’s decisions.
In
this study, the cards were presented to each patient who was asked to choose
the one that was closer to his/her preferences in a hypothetical scenario of a
consultation with their oncologist, when a decision about treatment must be
made. In this way, patients felt free to choose the role they really prefer to
play in the decision making process, without worrying about their physician’s
opinion. The CPS was translated from English to Greek by Almyroudi et al. [16].
Ethical approval was obtained from the research team that conducted the Greek
translation for the use of the CPS-Greek edition questionnaire.
Ethics
A
written authorization was obtained from the Ethics Committee and the Scientific
Council of the hospital that was chosen for the study. Patients were invited to
participate in the study and were then provided with additional information
about the research. Prior to the interview, patients who were recruited read
and signed information consent form. The research was conducted with respect to
the patients and the confidentiality of the collected data in accordance with
the Helsinki Declaration of 1975, as revised in 2013.
Statistical
Analysis
Continuous variables are presented with mean and Standard Deviation (SD) or with median and Interquartile Range (IQR). Qualitative variables are presented with absolute and relative frequencies. The Kolmogorov-Smirnov test and graphs (histograms and normal Q-Q plots) were used to test the normality of the distribution of the continuous variables. Demographic and clinical characteristics were independent variables while the role patients prefer to play in the decision-making process was the dependent dichotomous variable.
Bivariate analyses between demographic and clinical characteristics and the role patients prefer to play in the decision-making process included chi-square test, chi-square trend test, independent samples t-test and Mann-Whitney test. We used chi-square test in case of categorical demographic and clinical characteristics and chi-square trend test in case of ordinal variables. Also, we used independent samples t-test in case of continuous variables that followed normal distribution and Mann-Whitney test in case of continuous variables that did not follow normal distribution. Demographic and clinical characteristics with p<0.20 in bivariate analyses, were entered into the backward stepwise multivariate logistic regression analysis with the role patients prefer to play in the decision-making process as the dependent variable.
Multivariate analysis was used to control potential confounding variables. Criteria for entry and removal of variables were based on the likelihood ratio test, with enter and remove limits set at p<0.05 and p>0.05. We estimated adjusted odds ratios with 95% confidence intervals for the predictive factors related to the role patients prefer to play in the decision-making process. All tests of statistical significance were two-tailed, and P values of less than 0.05 were considered significant. The Statistical Package for Social Sciences (IBM SPSS) program, version 21.0. (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, version 21.0. Armonk, NY: IBM Corp.) was used for statistical analysis.
Results
Sample
Description
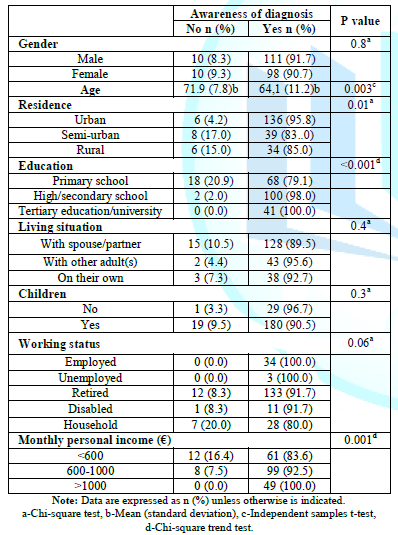
There were no complaints regarding the time of the completion and understanding of the questionnaire. Participants were mostly male (n=121), with an average age 64.8 years (SD=11.2). Most of the patients (n=102) were high/secondary school graduates and 46.7% of them (n=107) had a monthly personal income of 600-1.000€. Nearly one fifth of the patients (19.2%) were diagnosed with breast cancer and 18.8% (n=43) with lung cancer. The median duration of their Diagnose was 22.5 months (IQR: 1-128, SD: 28.3). Almost half patients (n=106) had no metastatic cancer, while 28.8% (n=66) of patients had undergone chemotherapy. Most of the participants were under therapeutical treatment (n=136), while 40.6% were under supportive treatment. Patients' demographic and clinical characteristics are presented in Table 1 and 2.
Awareness
of Diagnosis
As
shown in Table 1, the vast majority (91.3%) of study patients were aware of
their diagnosis being cancer. However, 20 patients reported that they did not
know their diagnosis. The mean age of patients who knew they suffer from cancer
was statistically significant lower than those who did not know (64.1 years
versus 71.9, p=0.003). Patients living in an urban area were significantly more
likely to know their diagnosis, compared to patients living in a semi-rural and
rural area (p=0.01). Higher educational level was statistical significantly
related to the patients’ knowledge of cancer diagnosis (p<0.001). Increased
monthly personal income was also statistically significant related to patient
awareness of diagnosis (p= 0.001).
The median duration of the disease of patients, who were aware of cancer diagnosis was statistically significantly higher than those who stated that they did not know their diagnosis was cancer (12 months versus 5, p=0.001). Patients with continuation/change of treatment were more likely to know they had cancer than those in the first cycle of treatment (p<0.001). Patients with no co-existing disease were significantly more likely to know they have cancer than those with a co-existing disease (p=0.03). In addition, all outpatients knew their diagnosis, while 14.4% of inpatients claimed they did know their diagnosis was cancer (p<0.001). Due to the variety of cancer diagnosis and the number of patients, Table 2 shows the most frequent cancer types of the study patients and the majority of the treatment combination they underwent.
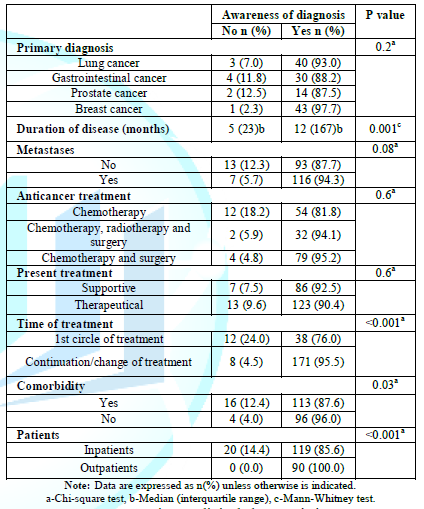
Table2:Patients’ clinical characteristics
Patients’
Decision-Making Preferences
As
shown in Table 3, 36.2% (n=75) of
patients chose to play a shared-decision role with their doctor in the decision-making
process. 33.3% (n=69) preferred their doctor to make the final decision
regarding treatment after taking the patient’s opinion seriously (passive
collaboration role), while only 0.5% (n=1) of patients chose to make all
decisions regarding treatment on their own (active role).
Bivariate analysis revealed the relationship between demographic and clinical characteristics of the study patients and their preferred role in the decision making process. Patients who chose the passive and passive/collaborative role constituted one category (passive role) (n=121), while patients who chose shared-decision, active/ collaborative and active role constituted the second category (non-passive role) (n=88). Dependent variable was the role patients prefer to play in the decision making process. Table 4 shortly represents the most important results of the analysis.
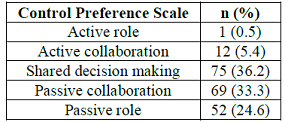
Table 3: Patients’ decision-making preferences
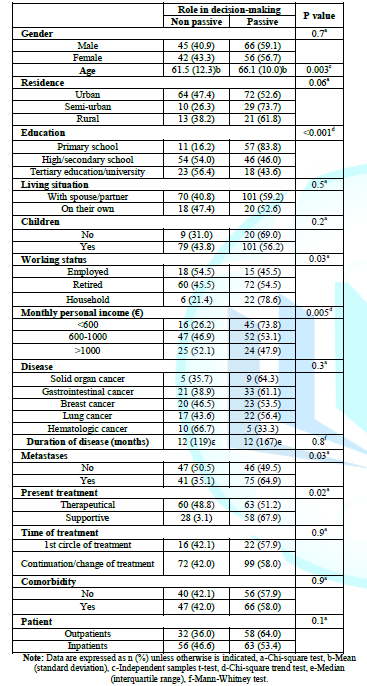
After the bivariate analysis, there was a statistically significant relationship (p<0.20) between the role patients prefer to play in the decision-making process and the age, residence, education, the existence of children, the occupational status, the monthly personal income, the existence of metastases, the type of treatment and the type of patients (outpatients/inpatients).
For this reason, multivariate regression analysis was conducted, with a dependent variable the role patients prefer to play in the decision-making process (non-passive role: reference category), the results of which are presented in Table 5.
The results of the multivariate regression analysis showed that older patients and those with lower educational level had an almost 1.04 and 2.63 times greater probability to adopt a passive role in decision-making procedures. The above variables interpret the 37% of the variability of passive role frequency volatility.
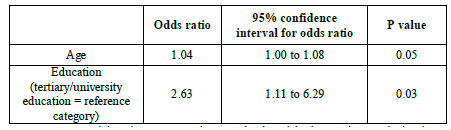
Table 5:Multivariate regression analysis with the patient
Discussion
The vast majority of the study patients knew their diagnosis was cancer (91.3%). Also, the largest percentage (57.9%) of them preferred to play a passive role in the decision-making procedures regarding cancer treatment. Both awareness of diagnosis and active/shared decision-making role were significantly associated with younger age and higher educational level.
Out of 229, 209 (91.3%) knew they suffered from cancer. Awareness of cancer diagnosis was found to be considerably associated with age, residence, educational level, and monthly personal income of the study patients. In particular, the elderly, patients who live in semi-rural and rural areas, patients with only compulsory education and those with an individual income of less than 600 euros per month were found to be unaware of cancer diagnosis in a higher rate. In a study on Greek cancer patients regarding awareness of cancer diagnosis conducted the previous decade found that 59% of cancer patients stated that they did not know their diagnosis [25]. Awareness of diagnosis was also significantly related to younger age and higher educational level, but also to female gender. In another study on Greek population in 2002, the percentage of patients who were unaware of cancer diagnosis was 63%. In this study, cancer patients who were mainly aware of their diagnosis were younger, high/secondary school or university graduates and suffering from breast cancer [6].
The Greek culture widely supports the ignorance of diagnosis in cancer patient, while the greater supporters of this phenomenon are the members of patients’ families. In Greece, family ties are particularly strong and family members share an intense feeling of offer and solidarity. Patients rely heavily on their family when they have serious problems and, above all, health problems, but relatives themselves usually experience patient health issues as a family issue and are actively involved in the process of dealing with the disease [31].
In the context of this protection, the fact that the diagnosis of cancer causes anxiety and sadness to patients, especially the elderly, who may feel helpless to cope with the disease’s challenges, relatives try to protect them by intervening and concealing not only the real diagnosis but even the type of the given treatment. This tactic, although still used nowadays, has gradually been replaced by the necessity of revealing the truth to cancer patients. A recent study in Turkey, where family ties are equally strong, shows that diagnosis has been hidden in cancer patients at high rates.
The reasons why patients' relatives conceal the diagnosis of cancer are to a great extent the anxiety and depression it may cause to sufferers. Specifically, in 129 newly diagnosed cancer patients, 29.5% had no knowledge of the diagnosis, while relatives claimed that revealing the truth would cause them severe psychological problems [32].
The same year in a study in India, where socio-cultural conditions and perceptions also seem to impede disclosure of diseases such as cancer, the vast majority of the cancer patients were unaware of their diagnosis. Specifically, only 29.9% of patients, most of them with non-small cell lung cancer and advanced disease knew they had cancer [33].
The previous decade in a study carried out in Norway, it was found that awareness of diagnosis of cancer patients was not certain. Specifically, 20% of study patients claimed that they did not know they had cancer. These patients were predominantly male, very young or elderly and smokers [34]. In a recent study in Philadelphia, it was found that the increased education level of cancer patients was significantly associated with increased level of awareness of cancer staging [35]. The study concluded that health professionals must recognize patients who require special attention due to their age or education level and evaluate whether they understood what their doctors explained to them regarding their disease and treatment.
On the other hand, revealing cancer diagnosis is an unpleasant process for healthcare professionals as well. Given the assumption that the disclosure of bad news may cause anxiety and sadness to patients their families, they choose to hide the diagnosis of cancer and ask the medical and nursing staff to do the same in an attempt to protect them [36,37]. Breaking bad news to cancer patients is causing a great anxiety to healthcare professionals, as they often do not know how to communicate the news with the patient, without causing sadness and unpleasant reactions. In addition, as it has been reported in previous studies, healthcare professionals have difficulty in using the appropriate language and understandable terms to simply and effectively explain to patients the details of their disease and treatment [38,39].
The disclosure of this truth has been a difficult process even for the most experienced doctors and nurses [40]. However, Greek healthcare professionals tend to increasingly adopt international models of disclosure to cancer patients, although this process remains particularly inconvenient and stressful for them [41,42].
It is, therefore, concluded that
awareness of diagnosis of cancer patients depend on different factors, which
are associated with health care professional as well as cancer patients and
their families.
As far as the patient's preferences in decision making procedure are concerned, the results of the statistical analysis showed that 36.2% of cancer patients want to co-decide with their doctor on their treatment, choosing the shared decision-making role. Only 5.8% of the patients preferred a more active role, while 57.9% preferred a more passive role, with 24.6% of them preferring a fully passive role, where the doctor takes all responsibility for the treatment decisions. Also, it was found that older and lower-educated patients preferred, in a higher rate, a more passive decision-making role. In line with the above, another study has been, recently, conducted on breast cancer patients in Greece. The majority of patients wished to have a passive role in the decision making process (71.1%), with most patients (45.3%) wanting their doctor to take full responsibility for cancer treatment decisions. The shared decision role was chosen by 24% of patients [16].
In a study among cancer patients, in Canada, the roles in the treatment decision making process patients preferred were 26% active, 25% passive and 49% collaborative. Older patients, women and Canadian patients than US patients were more likely to assume a passive role. Moreover, in a study in Switzerland, the vast majority of cancer patients (79.1%) agreed to the statement “one should stick to the physician advice even if one is not fully convinced of his idea”. Older patients and less educated patients were more likely to agree to this statement [29,43].
Arguably, older cancer patients have grown up in an era characterized by the “doctor-centered” model, which may help to explain their more passive role in the decision-making procedures. It was then believed that a patient would seem as “good customer”, trusting whatever the doctor suggested, without asking for more information or discuss treatment options [12]. Also, older patients might have lost hope, be depressed or overwhelmed by cancer-related symptoms and thus be unwilling to participate in the decision-making process [4]. On the other hand, patients with higher education level might have the ability to better access and understand medical information, which may affect patients’ preferred role in the decision-making procedure with the health care team. Knowledge is power and it is certainly easier for a patient with a good educational background to understand the doctor’s words, ask questions and make choices [44].
The rate at which Greek cancer patients choose a passive role in the decision making process is the highest compared to the corresponding percentage in both past and recent studies, internationally [45-56]. In a recent study in Spain, 21.2% of cancer patients receiving palliative care for their disease preferred a passive role in treatment decision process; while in the USA the percentage was still comparatively lower (13%) [57,58].
Many factors are likely related with the choice of passive role from Greek cancer patients. The paternalistic model of treatment decision-making, which is still largely prevalent in Greece, affects the counseling process with the health care team. Patients, usually, play a passive role in consultation and may have learned from past experiences that a more active role will not be easily accepted by healthcare professionals. Also, patients are likely to think that by choosing a more active role, they may seem recalcitrant patients and therefore not receive the proper care. Finally, apart from the paternalistic model in the doctor-patient relationship and the fear of the quality of care provided, the choices of Greek patients are likely to be influenced by their families, whose role is more intrusive in our country, resulting many times, as already mentioned, in concealing information from patients regarding diagnosis and the developments in their health status [16,41].
An additional factor that is not often mentioned but can greatly influence the degree to which patients will be involved in the decision making procedure is the enormous lack of time on behalf of healthcare professionals in order to allow time to further promote discussion and communication with the patients and their family members. In the recent years, hospitals in Greece are clearly under-staffed suffering serious shortages in both materials and building infrastructure, which causes serious problems in coordination, organization of time, and communication ultimately causing a reduction of the quality of holistic care provided to patients [41,59].
Active involvement of cancer patients in decision-making procedures regarding treatment requires a safe and calm environment, as well as healthcare professionals with high communication skills. The patients and their families should have adequate time to discuss with the healthcare team, share their concerns and express their wishes in order to make the appropriate decisions, with which they would feel comfortable, confident and satisfied. In addition, healthcare professionals should promote patients expression of possible changes in their decisions, as well as, the wish for further or detailed information regarding disease and treatment [60].
Therefore, the combination of inappropriate communication environment and the occupational exhaustion of doctors and nurses in Greek hospitals make it difficult for patients to participate in therapeutic decision-making in a more active way [41].
Strengths
This study concerns a rather underrated issue in Greece and a difficult issue to discuss with Greek patients. In Greek reality, almost the last two decades, the enormous lack of healthcare professionals, nursing staff and doctors along with the remaining hesitation of patients in getting the information they need for cancer diagnosis, derive them from their right to actively participate in decision-making procedures [16,18,27]. That is the reason why there are very few studies on the matter in Greece throughout the years. On the other hand, in Netherlands, researchers conducted a study about the preferences of cancer patients between two main treatments for early glottic cancer, which indicates that patients, in other countries in Europe, not only participate in decision making processes, nowadays, but also choose between treatments, when given a choice [61]. Therefore, the conduction of this study managed to provide health care professionals with the actual preferences of Greek cancer patients regarding their participation in decision-making and to emphases the need for better communication between health care professionals and cancer patients.
Limitations
This study had some limitations. The study sample consisted of patients suffering from various cancer types and the disease duration ranged from recent to many years. This may have confused patients about the therapeutic decisions they had taken, perhaps, several years ago and which could have changed over time. In addition the study sample was relatively small, which might affect the external validity of the study. Also, the study sample gathered from a single general hospital in Athens, which not only limited its number, but it might affected the results, since patients from purely cancer hospitals might be more aware of diagnosis and more active in the decision-making procedures. Perhaps, a multicenter study would have yielded more representative results and allow for additional correlations.
Conclusions
The results of the study showed that
Greek patients are more aware about cancer diagnosis, nowadays, but wish to
have a mainly passive and, to a lesser extent, a shared-decision role in the
decision-making procedures. This fact shows that the prevalent paternalistic
model of doctor-patient relationship in Greek reality may overshadow the
patients' actual needs and hinter the expression of their wishes or objections
to decisions regarding treatment.
This study, also, supports the need for a
unique and personalized patient care, at a time that in the country where the
study conducted, thousands of desperate people from different cultures are
flocking every day and the migration issue is a front line issue. Therefore,
even if the study results seem to address to Greek cancer patients, the truth
is that they apply to any cancer patient, who needs honest and person-centered medical
and nursing care and they could be included to cultural and migration patterns
round the world. Thus, health professionals should approach each patient and
his/her needs uniquely, by providing the appropriate information and options
available for cancer treatment, while being continuously alerted for signs of
intense anxiety and patient dissatisfaction.
References
- Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012 (2013) Inter J Can 136: 359-386. https://doi.org/10.1002/ijc.29210
- World Health Organization. 2017. Cancer.
- Eurostat Statistics Explained. 2017.
- Al Qadire M. Jordanian cancer patients’ information needs and information-seeking behaviour: A descriptive study (2014) Eur J Oncol Nurs 18: 46-51. https://doi.org/10.1016/j.pec.2004.06.006
- Rutten L, Arora N, Bakos A, Aziz N and Rowland J. Information needs and sources of information among cancer patients: a systemic review of research (2005) Patient Educ Couns 57: 250-261. https://doi.org/10.1016/j.pec.2004.06.006
- Iconomou G, Viha A, Koutras A, Vagenakis A and Kalofonos H. Information needs and awareness of diagnosis in patients with cancer receiving chemotherapy: A report from Greece (2002) Palliative Med 16: 315-321. https://doi.org/10.1191/0269216302pm574oa
- Rainey LC. Effects of preparatory patient education for radiation oncology patients (2006) Cancer 56: 1056-1061.
- Epstein RM and Street RL. Patient-centered Communication in Cancer Care: Promoting Healing and Reducing Suffering (2007) National Cancer Institute, NIH Publication, United States. https://doi.org/10.1037/e481972008-001
- Fallowfield L and Jenkins V. Communicating sad, bad and difficult news in medicine (2004) Lancet 363: 312-319. https://doi.org/10.1016/s0140-6736(03)15392-5
- Gordon EJ and Daugherty CK. “Hitting you over the head”: oncologists’ disclosure of prognosis to advanced cancer patients (2003) Bioethics 17: 142-168. https://doi.org/10.1111/1467-8519.00330
- Kaplowitz SA, Campo S and Chiu WT. Cancer patients’ desires for communication of prognosis information. Health Commun (2002) 14: 221-241. https://doi.org/10.1207/s15327027hc1402_4
- Leydon MG, Boulton M, Moynihan C, Jones A, Mossman J, et al. Cancer patients' information needs and information seeking behavior: in depth interview study (2000) BMJ 320: 909-913. https://doi.org/10.1136/bmj.320.7239.909
- Muthu Kumar D, Symonds RP, Sundar S, Ibrahim K, Savelyich BS, et al. Information needs of Asian and white British cancer patients and their families in Leicestershire: a cross-sectional survey (2004) Br J Cancer 90: 1474-1478. https://doi.org/10.1038/sj.bjc.6601774
- Seo M, Tamura K, Shijo H, Morioka E, Ikegame C, et al. Telling the diagnosis to cancer patients in Japan: attitude and perception of patients, physicians and nurses (2000) Palliat Med 14: 105-110. https://doi.org/10.1191/026921600676888353
- Bowling A and Ebrahim S. Measuring patients’ preferences for treatment and perceptions of risk (2001) Qual Health Care 10: 2-8.
- Almyroudi A, Degner L, Paika V, Pavlidis N and Hyphantis T. Decision-making preferences and information needs among Greek breast cancer patients (2011) Psy oncol 20: 871-879. https://doi.org/10.1002/pon.1798
- Institute of Medicine. Crossing the Quality Chasin: A New Health Care System for the 21st Century (2001) National Academies Press, United States.
- Alamanou GD, Balokas AS, Fotos VN, Patiraki E and Brokalaki H. Information needs of cancer patients: Validation of the Greek Cassileth’s Information Styles Questionnaire (2016) Eur J Oncol Nurs 20: 49-57. https://doi.org/10.1016/j.ejon.2015.11.002
- Matsuyama RK, Kuhn LA, Molisani A and Wilson-Genderson MC. Cancer patients’ information needs the first nine months after diagnosis (2013) Patient Educ Couns 90: 96-102. https://doi.org/10.1016/j.pec.2012.09.009
- Ankem K. Factors influencing information needs among cancer patients: A meta-analysis (2006) Libr Inf Sci Res 28: 7-23.
- Jenkins V, Fallowield L and Saul J. Information needs of patients with cancer: results from a large study in UK cancer centres (2001) Br J Cancer 84: 48-51. https://doi.org/10.1054/bjoc.2000.1573
- Rood J, Nauta I, Witte B, Stam F, van Zuuren F, et al. Shared decision-making and providing information among newly diagnosed patients with hematological malignancies and their informal caregivers: Not "one-size-fits-all" (2017) Psy oncol 26: 2040-2047. https://doi.org/10.1002/pon.4414
- Cardenas J, Infante P, Infante A, Chuang E and Selwyn P. Decisional Control Preferences in the Hispanic Population in the Bronx (2018) J Cancer Educ 34: 472-477. https://doi.org/10.1007/s13187-018-1325-9
- Brotons C, Björkelund C, Bulc M, Ciurana R, Godycki-Cwirko M, et al. Prevention and health promotion in clinical practice: the views of general practitioners in Europe (2005) Prev Med 40: 595-601. https://doi.org/10.1016/j.ypmed.2004.07.020
- Brokalaki E, Sotiropoulos G, Tsaras K and Brokalaki H. Awareness of diagnosis, and information-seeking behavior of hospitalized cancer patients in Greece (2005) Support Care Cancer 13: 938-942. https://doi.org/10.1007/s00520-005-0794-7
- Tsoussis S, Papadogiorgaki M, Markodimitraki E, Delibaltadakis G, Strevinas A, et al. Disclosure of cancer diagnosis: the Greek experience (2013) J BUON 18: 516-526.
- Bilanakis N, Vratsista A and Peritogiannis V. Preference for treatment Decision making among Greek medical patients (2015) Int J Emerg Ment Health 17: 341.
- Degner L, Sloan J and Venkatesh P. The control preference scale (1997) Can J Nurs Res 29: 21-43.
- Singh J, Sloan J, Atherton P, Smith T, Hack T, et al. Preferred roles in treatment decision making among patients with cancer: a pooled analysis of studies using the Control Preferences Scale (2010) Am J Manag Care 16: 688-696.
- Tariman J, Berry D, Cochrane B, Doorenbos A and Schepp K. Preferred and actual participation roles during health care decision making in persons with cancer: a systematic review (2010) Ann Oncol 21: 1145-1151. https://doi.org/10.1093/annonc/mdp534
- Alamanou D, Patiraki E and Brokalaki H. Information needs and decision-making preferences of cancer patients (2017) Hellenic J of Nursing 56: 211-219.
- Kalender ME, Bulbul F, Aktas G, Kus T, Okyar B, et al. Awareness of cancer diagnosis in Turkish patients can increase anxiety and depression: is it true? (2016) Ann Oncol 27: 1504. https://doi.org/10.1093/annonc/mdw390.72
- Aggarwal N, Singh N, Gupta D and Behera D. Does awareness of diagnosis influence health related quality of life in north Indian patients with lung cancer? (2016) Indian J Med Res 143: 38-44. https://doi.org/10.4103/0971-5916.191757
- Nord C, Mykletun A and Fosså SD. Cancer patients' awareness about their diagnosis: a population-based study (2003) J Public Health Med 25: 313-317. https://doi.org/10.1093/pubmed/fdg076
- Schaap A, Aggarwal R, Domogauer J. Patient awareness of staging in cancer diagnosis: Helpful or hurtful (2015) In: Proceedings of the 106th Annual Meeting of the American Association for Cancer Research, United States 18-22.
- Lee A and Wu HY. Diagnosis disclosure in cancer patients-when the family says "no!" (2002) Singapore Med J 43: 533-538.
- Lin HR and Bauer-Wu SM. Psycho-spiritual well-being in patients with advanced cancer: an integrative review of the literature (2003) J Adv Nurs 44: 69-80. https://doi.org/10.1046/j.1365-2648.2003.02768.x
- Friedrichsen MJ, Strang PM and Carlsson ME. Breaking bad news in the transition from curative to palliative cancer care- patient’s view of the doctor giving the information (2000) Support Care Cancer 8: 472-478.
- Wright EB, Holcombe C and Salmon P. Doctors’ communication of trust, care and respect in breast cancer: qualitative study (2004) BMJ 328: 864. https://doi.org/10.1136/bmj.38046.771308.7c
- Kawakami S, Arai G, Ueda K, Murai Y, Yokomichi H, et al. Physician's attitudes towards disclosure of cancer diagnosis to elderly patients: a report from Tokyo, Japan (2001) Arch Gerontol Geriatr 33: 29-36. https://doi.org/10.1016/S0167-4943(01)00099-1
- Mystakidou K, Tsilika E, Parpa E, Katsouda E and Vlahos L. Patterns and barriers in information disclosure between health care professionals and relatives with cancer patients in Greek society (2005) Eur J Cancer Care 14: 175-181. https://doi.org/10.1111/j.1365-2354.2005.00554.x
- Tsoussis S, Papadogiorgaki M, Markodimitraki E, Delibaltadakis G, Strevinas A, et al. Disclosure of cancer diagnosis: the Greek experience (2013) J BUON 18: 516-526.
- Langewitz W, Nubling M and Weber H. Hospital patients’ preferences for involvement in decision-making. A questionnaire survey of 1040 patients from a Swiss university hospital (2006) Swiss Med Wkly 136: 59-64.
- Say R, Murtagh M and Thomson R. Patients’ preference for involvement in medical decision making: A narrative review (2006) Patient Educ Couns 60: 102-114. https://doi.org/10.1016/j.pec.2005.02.003
- Beaver K, Luker K, Owens R, Leinster S, Degner L, et al. Treatment decision making in women newly diagnosed with breast cancer (1996) Cancer Nurs 19: 8-19. https://doi.org/10.1097/00002820-199602000-00002
- Degner L, Kristjanson L, Bowman D, Sloan JA, Carriere KC, et al. Information needs and decisional preferences in women with breast cancer (1997) J Am Med Assoc 277: 1485-1492.
- Wallberg B, Michelson H, Nystedt M, Bolund C, Degner L, et al. Information needs and preferences for participation in treatment decisions among Swedish breast cancer patients (2000) Acta Oncol 39: 467-476. https://doi.org/10.1080/028418600750013375
- Keating N, Guadagnoli E, Landrum M, Borgas C and Weeks JC. Treatment decision making in early-stage breast cancer: should surgeons match patients’ desired level of involvement? (2002) J Clin Oncol 20: 1473-1479. https://doi.org/10.1200/jco.2002.20.6.1473
- Lam W, Fielding R, Chan M, Chow L and Ho E. Participation and satisfaction with surgical treatment decision-making in breast cancer among Chinese women (2003) Breast Cancer Res Treat 80: 171-180. https://doi.org/10.1023/a:1024568732213
- Maly RC, Umezawa Y, Leake B and Silliman R. Determinants of participation in treatment decision-making by older breast cancer patients (2004) Breast Cancer Res Treat 85: 201-209. https://doi.org/10.1023/b:brea.0000025408.46234.66
- Jansen S, Ottew W and Stiggelbout A. Factors affecting patients’ perception of choice regarding adjuvant chemotherapy for breast cancer (2006) Breast Cancer Res Treat 99: 35-45. https://doi.org/10.1007/s10549-006-9178-z
- Sabo B, St-Jacques N and Rayson D. The decision-making experience among women diagnosed with stage I and II breast cancer (2007) Breast Cancer Res Treat 102: 51-59. https://doi.org/10.1007/s10549-006-9309-6
- Tyler Ellis C, Charlton ME and Stitzenberg KB. Patient-Reported Roles, Preferences, and Expectations Regarding Treatment of Stage I Rectal Cancer in the Cancer Care Outcomes Research and Surveillance Consortium (2016) Dis Colon Rectum 59: 907-915. https://doi.org/10.1097/dcr.0000000000000662
- Colley A, Halpern J, Paul S, Micco G, Lahiff M, et al. Factors associated with oncology patients' involvement in shared decision making during chemotherapy (2017) Psy oncology 26: 1972-1979. https://doi.org/10.1002/pon.4284
- Yennurajalingam S, Rodrigues LF, Shamieh OM, Tricou C, Filbet M, et al. Decisional control preferences among patients with advanced cancer: An international multicenter cross-sectional survey (2018) Palliat Med 32: 870-880.https://doi.org/10.1177/0269216317747442
- Hamelinck V, Bastiaannet E, Pieterse A, van de Velde C, Liefers GJ, et al. Preferred and Perceived Participation of Younger and Older Patients in Decision Making About Treatment for Early Breast Cancer: A Prospective Study (2018) Clinical Breast Cancer 18: 245-253.
- Noguera A, Yennurajalingam S, Torres-Vigil I, Parsons HA, Duarte ER, et al. Decisional control preferences, disclosure of information preferences, and satisfaction among Hispanic patients with advanced cancer (2014) J Pain Symptom Manage 47: 896-905. https://doi.org/10.1016/j.jpainsymman.2013.06.010
- Atherton P, Smith T, Singh J, Huntington J, Diekmann B,et al. The relation between cancer patient treatment decision-making roles and quality of life (2013) Cancer 119: 2342-2349. https://doi.org/10.1002/cncr.28046
- Alamanou GD, Fotos VN and Brokalaki-Pananoudaki H. Methods of providing information to patients with cancer and securing their informed consent (2017) Archives of Hellenic med 34: 151-164.
- PEBC’s Ovarian Oncology Guidelines Group. A systematic review of patient values, preferences and expectations for the treatment of recurrent ovarian cancer (2017) Gynecol Oncol 146: 392-398. https://doi.org/10.1016/j.ygyno.2017.05.039
- Van Loon Y, Hendriksma M, Langeveld TPM, de Jong MA, Baatenburg de Jong RJ, et al. Treatment Preferences in Patients with Early Glottic Cancer (2018) Ann Otol Rhinol Laryngol 127: 139-145.
*Corresponding author
Despoina G Alamanou, 2nd Internal Medicine Department, 417 NIMTS Hospital of Athens, Greece,Tel: +00306937509784, E-mail: despina_alamanou@hotmail.com
Citation
Alamanou DG, Giakoumidakis K, Theodosiadis DG, Fotos NV, Patiraki E, et al. Awareness of diagnosis and decision-making preferences of greek cancer patients (2020) Pharmacovigil and Pharmacoepi 3: 5-12.
Keywords
Cancer,
Decision-making, Diagnosis, Oncology, Patients' participation, Patients'
preferences, Role preference.


 PDF
PDF