Review Article :
Juan Simon Rico-Mesa, Stephanie Cornell and Rushit Kanakia Aspirin was once the mainstay of stroke prevention in
patients with atrial fibrillation. Its popularity was based on the results of
the SPAF and PATAF trials, which showed the low risks of this therapy and the
many benefits it had to offer in terms of embolic complications prevention.
Nevertheless, aspirin has lost popularity in atrial fibrillation since the
CHADS, CHA2DS2-VASc and HASBLED scoring systems were
first introduced. These scoring systems showed a different perspective, which
highlighted that thromboembolic risk varied among individuals and that a
generalization on antiplatelet therapy for atrial fibrillation was not
effective. These caveats gave support to additional treatments based on
anticoagulation, including warfarin and direct oral anticoagulants. These
treatments gained popularity based on the superiority over warfarin, first
described on the BAFTA trial, which nominated the warfarin as the standard of
care for atrial fibrillation thromboembolic prevention. Since then, direct
anticoagulation therapies have gained popularity based on the results of the
ARISTOTLE (apixaban), RE-LY (dabigatran), ROCKET-AF (rivaroxaban), ENGAGE TIMI
48 AF (edoxaban) trials. However, the CHA2DS2-VASc score
was generous with aspirin, since it opened a possible recommendation for low CHA2DS2-VASc
scores (0-1). This comprehensive literature review is intended to discuss the
arguments behind this last statement and to show the available evidence in
favor of and against aspirin for non-valvular atrial fibrillation in low
thromboembolic risk patients. Aspirin
was once the mainstay of stroke prevention in atrial fibrillation. However, the
development of Vitamin K Antagonists (VKAs) and the evolution and availability
of Direct Oral
Anticoagulants (DOACs), has left aspirin (ASA) therapy by the wayside,
based on the results of the BAFTA, ARISTOTLE, RE-LY and ROCKET-AF trials. Both
ASA as monotherapy and ASA as dual-antiplatelet therapy are no longer
recommended as first line stroke prevention in patients with CHA2DS2-VASc
≥ 2 [1,2]. Exceptions in the guidelines exist only in certain clinical settings,
particularly in those with CHA2DS2-VASc score=1 [3].
Besides primary outcomes, including endpoints such as cardiovascular death and
mortality, VKAs have additionally shown no increased risk of bleeding compared
to ASA, especially among the moderate to high-risk sub-group of atrial
fibrillation patients [4,5,6-9]. Regarding ASA use for cardiovascular benefit, ASA is
ineffective at increasing disability-free survival or at decreasing mortality
among healthy elderly adults without clear risk factors [10,11]. This calls
into question the popular assumption that the benefits of ASA therapy for cardiovascular
health of the general population outweigh negative side effects. Therefore, ASA
use overall should be carefully assessed, particularly in patients with atrial
fibrillation. Interestingly, even more than a decade after the first
generation of studies showing superiority of VKAs for stroke prevention in
atrial fibrillation, ASA continues to be prescribed to patients with CHADS2
scores of greater than or equal to 2 despite overwhelming evidence against,
based on the results of the PINNACLE trial, which involved 210,380 patients
with high CHADS2 scores [12]. In fact, in 2012 the European Society
of Cardiology
recommended ASA for patients who refused anticoagulation, consistent with
evidence at the time that ASA did have benefit over no therapy for this patient
population [13]. Regarding specifically lower risk patients, the 2014 American
College of Cardiology/American Heart Association guidelines recommend no
antithrombotic therapy or treatment with an oral anticoagulant or aspirin for
non-valvular atrial fibrillation with CHA2DS2-VASc=1 [2].
With a spotlight on ASA this year in the literature, it is appropriate to
re-evaluate ASA as alternative therapy to VKA or DOAC for patients with atrial fibrillation.
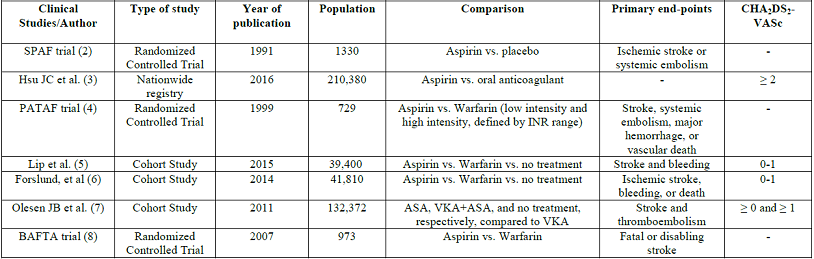
Specifically, evidence should be evaluated behind the benefit of ASA vs VKA or
DOAC vs no therapy for patients with non-valvular atrial fibrillation and CHA2DS2-VASc=0
or 1 (Table 1). The evidence for ASA for stroke prevention in patients with
atrial fibrillation with low risk of stroke (CHADSVASC<2) stems from the
Stroke Prevention in Atrial Fibrillation (SPAF) trial, published in 1991, which
followed patients for a mean of 1.3 years and found a 42% reduction in ischemic
stroke and embolism, as well as decreased mortality, with ASA compared to
placebo. Nevertheless, the SPAF trial also looked at warfarin outcomes and
found that warfarin had a superior reduction of primary events or death
compared to aspirin, 58% (p=0.01) vs. 32% (p=0.02). The risk of significant
bleeding was 1.5% vs. 1.4%, respectively [2]. Based on this early study, ASA
appeared to be a safe and effective (albeit less so) alternative to VKAs. Nevertheless, this study was performed in an era where
CHADSVASC had not been described before, and generalization among different
thrombotic risks and lack of standardized criteria was evident. Even though the
SPAF trial gave a hope for aspirin, evidence has been slowly proving it
differently. In 2000, the Primary Prevention of Arterial Thromboembolism in
Nonrheumatic Atrial Fibrillation (PATAF) trial supported the popular opinion
that ASA was an accessible and inexpensive therapy for those at low risk of stroke
or embolism, with a decreased risk of bleeding compared to anticoagulation and
a low drug-interaction
profile. It should be noted, however, that the PATAF trial was a relatively
small study of a uniform, elderly population in the Netherlands [14]. This study also found that ASA did not decrease risk of
bleeding compared to warfarin. Specifically, this study supported a neutral or
positive net clinical effect of warfarin over ASA in low risk patients with
atrial fibrillation, which contradicts the prior assumption that as risk
decreased, the efficacy of ASA increased enough to become clinically indicated
[16]. This study was the cornerstone for developing the most recent studies
that advocate for anticoagulation
over antiplatelet in CHA2DS2-VASc ≥ 1. Numerous other
studies throughout the last several decades also support either similar
bleeding risk or insignificant difference in bleeding risk between ASA and VKA
or between ASA and DOACs [4,5,6-8]. A Swedish study in 2014 also evaluated the risk of stroke or
embolism in atrial fibrillation. Their findings were consistent with a low
support of ASA in low risk patients, finding that patients with CHA2DS2-VASc
scores of 0-1 had a 1.0-1.2% one-year risk of ischemic stroke with ASA therapy
compared to a 0.1-0.2% risk without any treatment, which suggests that ASA
likely has no clinical benefit compared to no therapy for patients with low
risk of stroke or embolism [17]. It should be noted that both the
aforementioned Danish and this Swedish study were regional studies with
presumably homogenous populations, thus lacking external validity in other
populations and ethnicities. A recent study published in 2015 by Lip, et al. compared ASA
to warfarin therapy for primary prevention of stroke or embolism in those with CHA2DS2-VASc
scores of 0 or 1 [18]. They included a total of 39,400 patients, of which
10,475 were treated with VKAs; 5,353 were treated with ASA; and 23,572 were
left untreated. Primary endpoints, including stroke, bleeding and death, were
evaluated by both an intention-to-treat and Continuous Treatment analyses. The
authors found that for those with a low risk of stroke or embolism, defined as CHA2DS2-VASc=0
for males and CHA2DS2-VASc=1 for females, the risk of
stroke, bleeding, and death was truly low, and there was therefore no net
clinical benefit of treatment with either VKA or ASA. In those with one additional risk factor (CHA2DS2-VASc=1
for male and CHA2DS2-VASc=2 for female), ASA did not
significantly reduce risk of stroke and was significantly associated with
increased risk for
bleeding, i.e., regardless of sex, ASA therapy does not prevent stroke in
those with CHA2DS2-VASc=1, and furthermore does not
prevent stroke in women with CHA2DS2-VASc=2. However, in
untreated patients with one additional risk factor (CHA2DS2-VASc=1
for male and CHA2DS2-VASc=2 for female), 1-year stroke
risk increased by 3.01-fold, bleeding by 2.35-fold and death by 3.12-fold. The
authors also found that for those with one additional risk factor (CHA2DS2-VASc=1
for male and CHA2DS2-VASc=2 for female), there were
reductions in stroke and death with VKAs compared to no treatment and with VKAs
compared to ASA, without a significant increase in bleeding with VKA vs ASA
[18] . In the last three decades, ASA therapy has repeatedly been
found to be inferior to anticoagulation for preventing stroke in patients with
non-valvular atrial fibrillation, even for those with low risk of embolism or
stroke (CHA2DS2-VASc ≤ 1). Furthermore, ASA is not
associated with decreased risk of bleeding compared to VKA. The net benefit of
ASA therapy for these patients, therefore, does not have supporting evidence,
and we conclude that patients with low CHA2DS2-VASc
should not be offered ASA as a safer alternative to anticoagulation. Reasons to
prescribe ASA in this patient population include availability, financial
accessibility, and convenience, but these values are counterbalanced by similar
bleeding risk to VKA and significantly decreased efficacy at preventing the
primary outcome. 1. Ruff CT,
Giugliano RP, Braunwald E, Hoffman BE, Deenadayalu N, et al. Comparison of the
efficacy and safety of new oral anticoagulants with warfarin in patients with
atrial fibrillation: A meta-analysis of randomised trials (2014) The Lancet
383: 955-962. https://doi.org/10.1016/S0140-6736(13)62343-0
2. January
CT, Wann LS, Alpert JS, Calkins H, Cigarroa EJ, et al. 2014 AHA/ACC/HRS guideline
for the management of patients with atrial fibrillation: A report of the
american college of cardiology/american heart association task force on
practice guidelines and the heart rhythm society (2014) J Am Coll Cardiol 64:
e1-e76. https://doi.org/10.1016/j.jacc.2014.03.022
3. Valgimigli
M, Bueno H and Byrne RA. 2017 ESC focused update on dual antiplatelet therapy
in coronary artery disease developed in collaboration with EACTS (2017) Eur J
cardio-thoracic sur 53: 34-78. https://doi.org/10.1093/eurheartj/ehx638
4. Stroke
prevention in atrial fibrillation study: Final results (1991) Circulation 84:
527-539. https://doi.org/10.1161/01.CIR.84.2.527
5. Mant J,
Hobbs FR, Fletcher K, Roalfe A, Fitzmaurice A, et al. Warfarin versus aspirin
for stroke prevention in an elderly community population with atrial
fibrillation (the birmingham atrial fibrillation treatment of the aged study,
BAFTA): A randomised controlled trial (2007) The Lancet 370: 493-503. https://doi.org/10.1016/S0140-6736(07)61233-1
6. Adjusted-dose
warfarin versus low-intensity, fixed-dose warfarin plus aspirin for high-risk
patients with atrial fibrillation: Stroke prevention in atrial fibrillation III
randomised clinical trial (1996) The Lancet 348: 633-638. https://doi.org/10.1016/S0140-6736(96)03487-3
7. Albers
GW, Dalen JE, Laupacis A, Manning WJ, Petersen P, et al. Antithrombotic therapy
in atrial fibrillation (2001) Chest-Supplements 119: 194S-206S. https://doi.org/10.1378/chest.119.1_suppl.194S
8. Hart RG,
Pearce LA and Aguilar MI. Meta-analysis: Antithrombotic therapy to prevent
stroke in patients who have nonvalvular atrial fibrillation (2007) Ann Intern
Med 146: 857-867. https://doi.org/10.1016/j.pcad.2015.07.003
9. Potpara
TS and Lip GY. Oral anticoagulant therapy in atrial fibrillation patients at
high stroke and bleeding risk (2015) Prog Cardiovasc Dis 58: 177-194. https://doi.org/10.1016/j.pcad.2015.07.003
10. McNeil JJ,
Woods RL, Nelson MR, Reid CM, Kirpach B, et al. Effect of aspirin on
disability-free survival in the healthy elderly (2018) N Engl J Med 379:
1499-1508. 11. McNeil JJ,
Nelson MR, Woods RL, Lockery JE, Wolfe R, et al. Effect of aspirin on all-cause
mortality in the healthy elderly (2018) N Engl J Med 379: 1519-1528. 12. Hsu JC,
Maddox TM, Kennedy K, Katz FD, Marzec NL, et al. Aspirin instead of oral
anticoagulant prescription in atrial fibrillation patients at risk for stroke
(2016) J Am Coll Cardiol 67: 2913-2923. https://doi.org/10.1016/j.jacc.2016.03.581
13. Camm AJ,
Lip GY, De Caterina R, Savelieva I, Atar D, et al. 2012 focused update of the
ESC guidelines for the management of atrial fibrillation: An update of the 2010
ESC guidelines for the management of atrial fibrillation developed with the
special contribution of the european heart rhythm association (2012) Eur Heart
J 33: 2719-2747. https://doi.org/10.1093/eurheartj/eht291
14. Hellemons
BS, Langenberg M, Lodder J, Schouten HJA, Van Ree JW, et al. Primary prevention
of arterial thromboembolism in non-rheumatic atrial fibrillation in primary
care: Randomised controlled trial comparing two intensities of coumarin with
aspirin (1999) BMJ 319: 958-964. https://doi.org/10.1136/bmj.319.7215.958
15. Connolly
S, Pogue J, Hart R, Pfeffer M, Hohnloser S, et al. Clopidogrel plus aspirin
versus oral anticoagulation for atrial fibrillation in the atrial fibrillation
clopidogrel trial with irbesartan for prevention of vascular events (ACTIVE W):
A randomised controlled trial (2006) Lancet 367: 1903-1912. https://doi.org/10.1016/S0140-6736(06)68845-4
16. Olesen JB,
Lip GY, Lindhardsen J, Lane AD, Ahlehoff O, et al. Risks of thromboembolism and
bleeding with thromboprophylaxis in patients with atrial fibrillation: A net
clinical benefit analysis using a real world nationwide cohort study (2011)
Thromb Haemost 106: 739-749. https://doi.org/10.1160/TH11-05-0364
17. Forslund
T, Wettermark B, Wändell P, von Euler M, Hasselström J, et al. Risks for stroke
and bleeding with warfarin or aspirin treatment in patients with atrial
fibrillation at different CHA2DS2-VASc scores: Experience
from the stockholm region (2014) Eur J Clin Pharmacol 70: 1477-1485. https://doi.org/10.1007/s00228-014-1739-1
18. Lip GY,
Skjøth F, Rasmussen LH and Larsen TB. Oral anticoagulation, aspirin, or no
therapy in patients with nonvalvular AF with 0 or 1 stroke risk factor based on
the CHA2DS2-VASc score (2015) J Am Coll Cardiol 65:
1385-1394. https://doi.org/10.1016/j.jacc.2015.01.044
Juan Simon Rico-Mesa, Department of Medicine, Division of Internal Medicine,
University of Texas Health San Antonio, USA, E-mail: mesajs@uthscsa.edu Rico-Mesa SJ, Cornell S and Kanakia R. Current evidence for the use of
aspirin in patients with atrial fibrillation and a CHA2DS2-VASc=1
(2019) Clinical Cardiol Cardiovascular Med 3: 7-9. Atrial fibrillation, Anticoagulation therapies,
Cardiovascular health.Current Evidence for the Use of Aspirin in Patients with Atrial Fibrillation and a CHA2DS2-Vasc=1
Abstract
Full-Text
Background
The
Evidence
More recently, a meta-analysis published in 2007 supported these early
findings. Hart et al. concluded that ASA did reduce risk of stroke and embolism in
patients with atrial fibrillation by 20% compared to placebo, in addition to a
similar decrease in mortality. Nonetheless, warfarin was found to reduce stroke
by 60%. Of note, this meta-analysis included patients with both low and high CHA2DS2-VASc
values. Sub-group analysis was not performed, so conclusions for low vs high CHA2DS2-VASc
values were not assessed. Most studies included in this meta-analysis
specifically targeted primary prevention [15]. In 2011, a large study in
Denmark performed sub-group analyses of VKA vs ASA vs placebo by CHADS2
and CHA2DS2-VASc scores. The results showed no net
clinical benefit of ASA in patients with a low risk of stroke or embolism
(CHADS ≥ 0 or CHA2DS2-VASc ≥ 1). Conclusion
References
*Corresponding
author:
Citation:
Keywords