Research Article :
Kazi Zahidul Hoque, Masumul Gani Chowdhury,
Ashraful Islam, Makbul Hossain, Mostafizur Rahman, Sohail Ahmed and Mohammed
Zakir Hossain Background: Ventricular Septal Defect (VSD) is the commonest congenital cardiac anomaly in Bangladesh. For this reason, patch repair of VSD is commonly performed cardiac surgery here. Aim: To observe the short term outcome of patch repair of VSD. Methods: 50 consecutive patients were enrolled in the study by purposive sampling who received treatment for isolated VSD in Department of Paediatric Cardiac Surgery of Dhaka Shishu Hospital, Dhaka, Bangladesh. They underwent ventricular patch repair from January, 2017 to December, 2017. A prospective observational cross-sectional study was conducted for this 12 months period. A pre-structured, interview and observation based, peer reviewed data collection sheet was prepared. Data regarding Sociodemographic, clinical, surgical and outcome profile were recorded. Data were compiled, edited and analyzed with SPSS version 23. Data were presented as mean and standard deviation, frequency percentage and median with range. Results: The mean birth weight of 50 patients was 2.8 kg (range: 2.1-3.5 kg) whereas the median of gestational age was 38 weeks. Among these 50 patients, 22 (44%) and 28 (56%) were boys and girls respectively. The indication of surgery was volume load, failure to thrive and repeated respiratory tract infection. Out of 50 patients, 46 (92%) had perimembranous variety. On the contrary, 4 (8%) experienced Double committed type of VSD. The mean Bypass time and Aortic cross-clamp time were recorded as 70 ± 13.7 minutes and 35 ± 6.85 minutes respectively. Out of 50 patients who underwent ventricular patch repair, 2 (4%) experienced pneumothorax, 1 (2%) got chylothorax and 1 (2%) had transient heart block. Total 45 (90%) patients showed uneventful outcome. Conclusion: Contemporary results of ventricular patch repair in case of VSD showed unparallel outcome with extremely low morbidity in our perspective. Congenital
heart disease is a spectrum of structural problems of the heart or its
major blood vessels which are present at birth due to failure of embryological
development of fetus in the womb. VSD accounts for about 14-16% of all cases of
congenital cardiovascular defects [1]. About eight of every 100 infants or 1%
of live births is born every year with congenital cardiovascular defects. It is
the number one cause of death from birth defect during the first year of life
[1]. The defects can exist in isolation, can be complicated by additional
intracardiac lesions, or can be part of more complex combinations, such as
tetralogy of Fallot, double outlet right ventricle, transposition, or
functionally univentricular hearts. There are 4 subgroups defined in the guidelines, according to
defect location: perimembranous, muscular, outlet and inlet type. The
perimembranous type is the most frequent (about 80% of all VSDs) among adult
population [2]. The clinical presentation and natural history can vary from
small VSD with insignificant left-to-right shunt to VSD with significant
left-to-right shunt with Left Ventricular (LV) volume overload and Right
Ventricular (RV) pressure overload, which, if unrepaired, may cause pulmonary
vascular disease and even Eisenmenger syndrome [3,4].
Patients with a small VSD and insignificant left-to-right shunt or with a
repaired VSD usually remain event-free during follow-up. However, several problems may still develop later in life,
with the most important being endocarditis, LV dilatation due to volume
overload, double-chambered right ventricle, Left Ventricular Outflow Tract
Obstruction (LVOTO), Aortic
Valve Regurgitation (AR) and complete heart block (especially in the earlier
years of cardiac surgery) [2]. Though spontaneous closure in the first years of
life is anticipated in cases of small defect; surgical repair is the gold
standard treatment of VSD still yet. The main aim of this study is to observe
the short term outcome of patch repair of VSD. This study was conducted in Department of Pediatric Cardiac Surgery
of Dhaka Shishu Hospital from May, 2017 to December, 2017. It is a prospective
observational study. Initially all the patients admitted for VSD repair were
enrolled by purposive sampling. The complicated cases where other congenital
major deformities present were excluded from the study. A simple VSD which can
be defined as an isolated VSD or a VSD with concomitant Atrial Septal Defect
(ASP)/Patent Foramen
Ovale (PFO), Patent Ductus Arteriosus (PDA) or mildly stenotic/regurgitant
semilunar valves patients were included in this study. At first, 56 patients were enrolled. Among them we kept only
50 patients according to the eligibility criteria. We prepared a
pre-structured, peer-reviewed, interview and observation based data collection
sheet. And we recorded pre, peri and postoperative data including
sociodemographic, neonatal, on admission and perioperative clinical,
biochemical and surgical variables. Surgical outcome and complications were
assessed according to international criteria [5]. Primary objectives were to
see immediate post-operative out-come, the number of ICU stay, Inotrope support
and secondary objectives were to see any major post-operative complications. Safety
parameters are also included, like the selection of the patient without any
pre-operative infections, other major congenital
malformations, lack surgeons experience and post-operative ICU care. All data were recorded, managed and analyzed with the help of
Statistical Packages for Social Science (SPSS) version 23 (Ilinois, Chicago,
USA). Frequencies and percentages were used for the qualitative variables
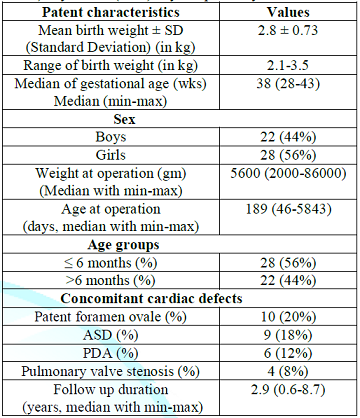
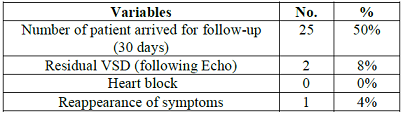
median was used for data which were not normally distributed. Table 1 shows that
the overall characteristics of patents where the mean birth weight and median
weight at operation were 2.8 ± 0.73 kg and 5600 gram. Among 50 children, there
were 22 (44%) boys and 28 (56%). On the contrary, 28 (56%) patients were in the
group of ≤ 6 months and 22 (44%) patents were in the group of >6 months
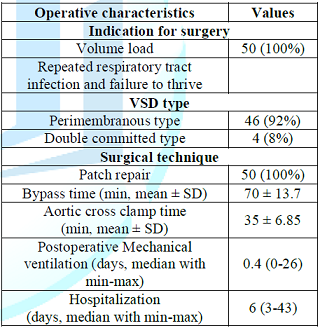
during operation. Table 2 shows that
all 50 patients underwent patch repair due to volume load, repeated RTI and
Failure to thrive in VSD. There were 2 types of VSD in this series. Out of 50
patent 46 (92%) had perimembranous type and 4 (8%) had double committed type. The mean bypass and aortic cross clamp time was 70 ± 13.7
minutes and 35 ± 6.85 minutes respectively. The median postoperative mechanical
ventilation duration and hospitalization duration were 0.4 (range: 0-26) days
and 6 (3-43) days respectively. Table 1:
Distribution of patients according to different characteristics (N=50). Table 2: Operative
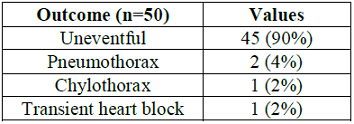
characterizes (N=50). Table 3 shows that
out of 50 patients with patch repair for VSD, 45 (90%) showed uneventful
outcome whereas 2 (4%) patients suffered from post-operative pneumothorax. On
the contrary, 1 (2%) patient each experienced chylothorax and transient heart
block after surgery. Table 3:
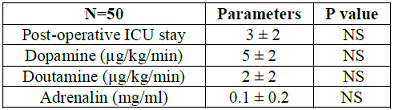
Distribution of patients according to outcome (N=50). Table 4: Immediate
Post-operative ICU parameters. Table 5: Post-Operative
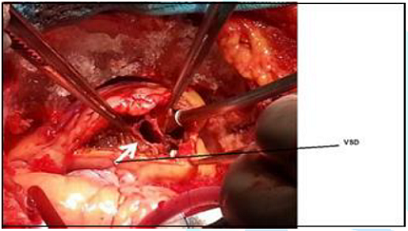
Follow-up after discharge. To perform intracardiac repair of VSD, median sternotomy was
performed in all patients. All patients underwent cardiopulmonary bypass. Three
surgeons from the different hospitals across the country performed the
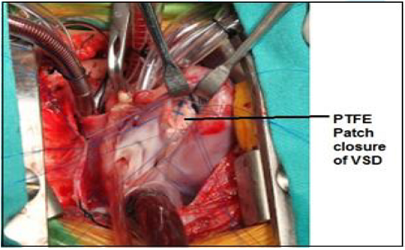
surgeries (Two surgeons performed 97.5% of the surgeries). We performed PTFE
patch closure of all VSD, not a single direct closure was done. Concomitant
closure of atrial septal defect closure, patent foramen ovale closure, patent ductus arteriosus
ligation, infundibular muscle resection, valvuloplasty and/or division was
done when needed. We selected the patients based on clinical symptoms and
transthoracic Echocardiography, only one patient was checked for reversible
pulmonary arterial hypertension by cardiac cath. After the operation on one
Post-operative day, we performed a Transthoracic
Echocardiogram to check the result. Before discharge another transthoracic
Echocardiogram was performed in all cases (Figure
1 and 2). Figure 2: PTFE patch
closure of VSD through right atriotomy. VSDs arise from failure of growth, alignment or fusion of one
or more septal components and are best classified according to their margins
and location [6]. A ventricular septal defect is a cardiac anomaly consisting of
a connection between the right ventricle and the left ventricle. These defects
can be single or multiple. A VSD may occur in any portion of the
interventricular septum, including the membranous, muscular, inlet, or outlet
septum, or a combination of locations. Perimembraneous VSD is
the most common type of VSD (80%). Part of the defect is bordered by the
fibrous continuity between the mitral and tricuspid valve. The defect may be
partially or completely occluded by the septal leaflet of the tricuspid valve. Muscular VSD is completely surrounded by muscular tissue.
These defects are by definition located in the muscular part of the ventricular
septum. Spontaneous closure of muscular VSDs frequently occurs in the first two
years of life. Outlet VSD is formed by the continuity between the aortic and pulmonary
valves. In this study, the mean birth weight of the respondents was 2.8 ± 0.73kg
which was lower than the similar Dutch study where the mean birth weight was
found, 3.14 (± 7.78) gm [7]. It was anticipated as the average growths of the
neonates of Dutch countries are more standard than us due to average maternal
nutritional deficit in our mothers in pregnancy. On the contrary, the median weight at operation in our
respondents was 5650 gm (range: 2000-86,000). The mean age at operation in the
study of Saudi Arabia was higher than our reports [8]. The median age at
operation in our aspect was 189 days (range: 46-5843 days). The similarities in
the results were not observed in the previous study of Saudia Arabia where mean
age at operation was higher [8]. It may be due to the poor performance status
of our children. In our study, PFO (20%), ASD (18%), PDA (12%) and Pulmonary Valve Stenosis
(PVS) (8%) were found as concomitant cardiac defect. These statistics were
almost consistent with previous study. Our all patients underwent patch repair where volume load,
repeated respiratory tract infection and failure to thrive are the indications
of surgery. There was no mortality observed in this study whereas major
morbidity like pneumothorax (4%), chylothorax (2%) and transient heart block
(1%) which was resolved within 7 days post operatively compare to Maartje, et
al. study where it was 4.9% completed heart block was observed, which was 8% on
that study, and other study showed it was 0.0-2.1% [9,10]. Outcome showed that
90% cases uneventful. However, ICU stay was 1-5 days, and some of them needed
inotropic support in different doses. Mostly inotropes are used, dopamine,
dobutamine and adrenaline, milrinone was not required. In the previous other
studies the complications related to VSD repair were observed for less than the
present report [11-13]. Three studies were conducted in the dedicated high
volume centers where logistic supports are more modernized than our center. Post-operative follow-up was the most challenging part,
because patients were reluctant to visit due to low socioeconomic condition.
Only 25 (50%) patients appeared on first 30 days follow-up. We havent included
later follow-up periods in this study. Out of them post-operative
Echocardiography shows 2 (8%) small residual VSD, expected to close
spontaneously on later date, no complete heart block was observed. And 2 (4%)
patients showed reappearance of symptoms, that is developed repeated
respiratory tract infection, and congestive heart failure,
for them dose of the drugs was adjusted accordingly. Being a developing country and poor socioeconomic status of
the patient, the follow-up was quite challenging and also sample number was too
little to come up a definitive conclusion. In Bangladesh perspective where pediatric cardiac surgery is
gradually gaining the popularity, there results can be claimed as excellent
with no mortality and manageable morbidity. 1.
Figueroa JDR, Magaña BDP, Hach JLP, Jiménez CC and
Urbina CR. Heart malformation in children with Down syndrome (2003) Rev Esp
cardiol 56: 894-899. https://doi.org/10.1016/S0300-8932(03)76978-4 2.
Baumgartner H, Bonhoeffer P, De Groot NM, de Haan F,
Deanfield JE, et al. ESC guidelines for the management of grownup congenital
heart disease (2010) Eur Heart J 31: 2915-2957. https://doi.org/10.1093/eurheartj/ehq249 3.
Penny DJ and Vick GW. Ventricular septal defect (2011)
Lancet 377: 1103-1112. https://doi.org/10.1016/s0140-6736(10)61339-6
4.
Soufflet V, de Bruaene VA, Troost E, Gewillig M, Moons
P, et al. Behavior of unrepaired perimembranous ventricular septal defect in
young adults (2010) Am J Cardiol 105: 404-407. https://doi.org/10.1016/j.amjcard.2009.09.047
5.
Jacobs ML, OBrien SM and Jacobs JP. An empirically
based tool for analyzing morbidity associated with operations for congenital
heart disease (2013) J Thorac Cardiovasc Surg 145: 1046-1057. https://doi.org/10.1016/j.jtcvs.2012.06.029
6.
Soto B, Becker AE, Moulaert AJ, Lie JT and Anderson
RH. Classification of ventricular septal defects (1980) Br Heart J 43: 332-343.
http://dx.doi.org/10.1136/hrt.43.3.332 7.
Schipper M, Slieker MG, Schoof PH and Breur PM. Surgical
Repair of Ventricular Septal Defect; Contemporary Results and Risk Factors for
a Complicated Course (2017) Pediatr Cardiol 38: 264-270. https://doi.org/10.1007/s00246-016-1508-2
8.
Ismail SR, Dughiem A, Abusuliman A, Kabbani M and Najm
N. 803 Effect of Body Weight on the Outcome of Ventricular Septal Defect Repair
(2012) Arch Dis Child 97: A230-A231. https://doi.org/10.1136/archdischild-2012-302724.0803
9.
Maartje S, Martijn GS, Paul HS and Johannes MPJB.
Surgical Repair of Ventricular Septal Defect; Contemporary Results and Risk
Factors for a Complicated Course (2017) Pediatr Cardiol 38: 264-270. https://doi.org/10.1007/s00246-007-9016-z
10.
Scully BB, Morales DL, Zafar F, McKenzie ED, Fraser CD,
et al. Current expectations for surgical repair of isolated ventricular septal
defects (2010) Ann Thorac Surg 89: 544-549. https://doi.org/10.1016/j.athoracsur.2009.10.057 11.
Scully BB, Morales DL, Zafar F, McKenzie ED, Fraser CD
Jr, et al. Current expectations for surgical repair of isolated ventricular
septal defects (2010) Ann Thorac Surg 89: 544-549. https://doi.org/10.1016/j.athoracsur.2009.10.057
12.
Anderson BR, Stevens KN and Nicolson SC. Contemporary
outcomes of surgical ventricular septal defect closure (2013) J Thorac
Cardiovasc Surg 145: 641-647. https://doi.org/10.1016/j.jtcvs.2012.11.032
13.
Kogon B, Butler H, Kirshbom P, Kanter K and McConnell
M. Closure of symptomatic ventricular septal defects: how early is too early? (2008)
Pediatr Cardiol 29: 36-39. https://doi.org/10.1007/s00246-007-9016-z Kazi Zahidul Hoque, Assistant Professor (Consultant) and Unit
Chief, Pediatric Cardiac Surgery Unit 2, Dhaka Shishu (Children) Hospital and
Institute of Child Health, Consultant, Metropolitan Medical Center, Dhaka 1207,
Bangladesh, Tel: +8801711352549, E-mail: kzhoque72@yahoo.com
Hoque ZK, Chowdhury GM, Islam A, Hossain M,
Rahman M, et al. Surgical repair of VSD and their short term outcome in a
tertiary care hospital (2019) Clinical Cardiol Cardiovascular Med 3: 34-37. Ventricular Septal Defect, Pediatric Cardiology,
Cardiac complications.Surgical Repair of VSD and their Short Term Outcome in a Tertiary Care Hospital
Abstract
Full-Text
Introduction
Materials
and Methods
Data Analysis
Results
Surgical
Technique
Discussion
Limitations
of the Study
Conclusion
References
*Corresponding
author:
Citation:
Keywords