Research Article :
Yasser Mohammed Hassanain Elsayed The initial
presentation of a novel Coronavirus-2 (COVID-19) that is resulting in Severe
Acute Respiratory Syndrome (SARS) had appeared in Wuhan, China in December 2019
[1]. COVID-19 Disease is a highly communicable, rapidly spread, lethal
worldwide disease [2]. Despite COVID-19 disease was primarily presented with
respiratory symptoms, but cardiovascular involvements were common and
accompanied by higher mortality among these patients [3]. However, cardiac
manifestations represent a late phenomenon of the viral respiratory infection
in COVID-19 patients. Myocardial infarction, arrhythmias, cardiac arrests,
Heart Failure (HF), and Venous Thromboembolism (VTE) are frequent
cardiovascular complications in COVID-19 patients that is varying from 7.2% up
to 33% [3]. Arrhythmias are commonly recognized sequel in COVID-19 patients,
with Atrial Fibrillation (AF) being the most common form. An electrical,
calcium handling and structural remodeling have represented keystone in
understanding AF pathogenesis [4]. The clinical
manifestations of AF are highly variable and the actual mechanisms of AF are
still vague in a big sector of patients [5]. The underlying pathogenesis of AF
in COVID-19 patients is still idiopathic [4]. According to current literature,
AF was detected in 19% to 21% among COVID-19 patients [4]. The incidence of AF
is usually high in patients with severe pneumonia, SARS, septic shock, and the
during hospitalization [4]. According to the Danish Nationwide Registry (DNR),
new-onset AF was reduced by 47% in the first three weeks of the national
lockdown in comparison with the simultaneously the past year [6]. A reduction
in angiotensin-converting enzyme 2 (ACE-2) receptor availability, CD147 and
sialic acid-spike protein reaction, increased inflammatory signaling
subsequently culmination in an inflammatory cytokine storm, direct viral
endothelial damage, acute electrolytes disturbance, acute acid-base imbalance,
and increased adrenergic drive are proposed putative mechanisms in the
pathophysiology of COVID-19 related-AF [7]. Currently, therapy of
AF with Antiarrhythmic Drugs (AADs), and anticoagulants are complex,
suboptimal, and are accompanied by anxious side effects [4]. Acute Coronary
Syndrome (ACS) due to a Coronary Artery Spasm (CAS) can occur in a severe acute
respiratory syndrome in COVID-19 patients [8]. Despite the actual mechanisms of
CAS in COVID-19 patients are multifaceted, but, it still unknown.
Hypercontractillity of coronary smooth muscle is usually induced by a rise of
IC calcium (CA++) especially with elevated CA++ sensitivity are proposed
mechanisms in understanding COVID-19 virus-inducing CAS [8]. However, CAS may
occur in patients with established atherosclerotic coronary lesions.
Importantly, inflammatory processes, IL-6 polymorphism, and oxidative stress
may implicate in the pathogenesis of COVID-19 virus-inducing CAS [9]. Moreover,
a major systemic inflammatory response, endothelial dysfunction, and activation
of the ACE-2 receptor may play a role in inducing coronary artery spasm in COVID-19
infection [10]. Wavy triple an
electrocardiographic sign (Yasser Sign) is a new innovated diagnostic sign in hypocalcaemia
[11]. The author interpretations for this sign are based on the following; So, this arrangement is
non-conditional. This is meaning the sign conditionally no affect specific ECG
partition e.g., inferior, anterior, or lateral, etc. Mostly, there is no
participation among the involved leads. Thus, the sign is not conditionally
included in an especial coronary artery for the affected leads [11]. A 60-year-old married
male, farmer, Egyptian patient presented to the Physician Outpatient Clinic (POC)
with acute tachypnea, chest pain, and palpitations. Fatigue, loss of appetite,
and generalized body aches were associated symptoms. He gave a history of
tachypnea for 4 days. Informed consent has been signed by the patient but
unfortunately, there was no ethical approval. Currently, he had a history of
contact in the past 7 days with his son who confirmed a COVID-19 patient. Upon
general physical examination; generally, the patient was tachypneic,
distressed, with an irregular pulse rate (atrial fibrillation of VR of 160),
blood pressure (BP) of 140/80 mmHg, respiratory rate of 40 bpm, the temperature
of 39.5°C, and pulse oximeter of oxygen (O2) saturation
of 88%. He seemed thin and long. No more relevant clinical data were noted
during the physical examination. The patient was treated
at home with COVID-19 pneumonia, atrial fibrillation, coronary spasm, and Wavy
triple sign or Yasser’s sign. Initially, the patient was treated with O2
inhalation by O2 cylinder (100%, by nasal cannula, 5L/min). The
patient was maintain treated with cefotaxime; (1000 mg IV every 8hours),
azithromycin (500 mg PO single daily dose), oseltamivir (75 mg PO twice daily
only for 5 days), and paracetamol (500 mg IV every 8 hours as needed). SC
enoxaparin 80 mg twice daily), aspirin tablet (75 mg, once daily), clopidogrel
tablet (75 mg, once daily), diltiazem tablet (60 mg, once daily), and
hydrocortisone sodium succinate (100 mg IV every 12 hours) were added. The
patient was daily monitored for temperature, pulse, blood pressure, and O2
saturation. The initial ECG on presentation showing atrial fibrillation (of VR
of 160) with a T-wave inversion in inferior leads (II, III, and aVF), in
anterior leads (V4-6 leads), and an upright T-wave in aVR lead. There is a Wavy
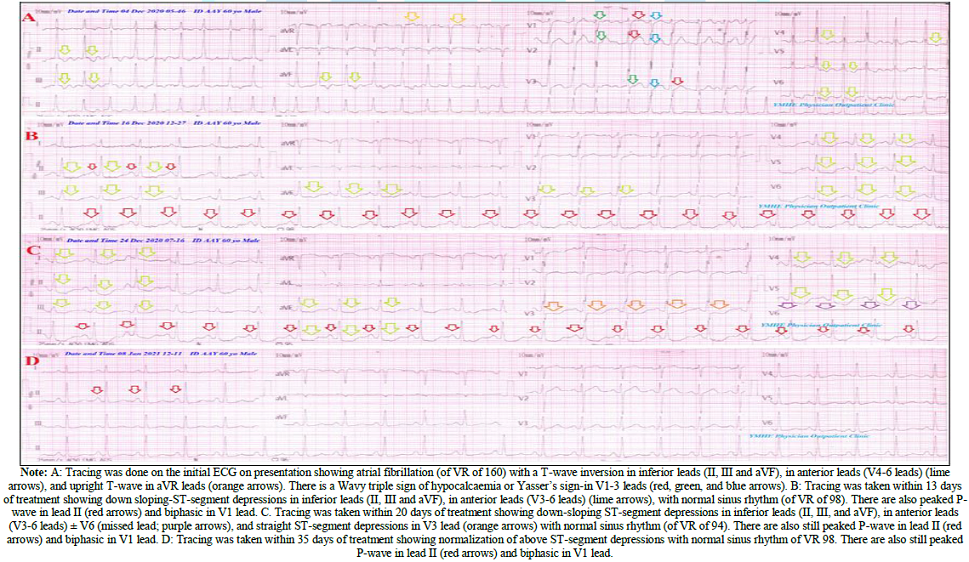
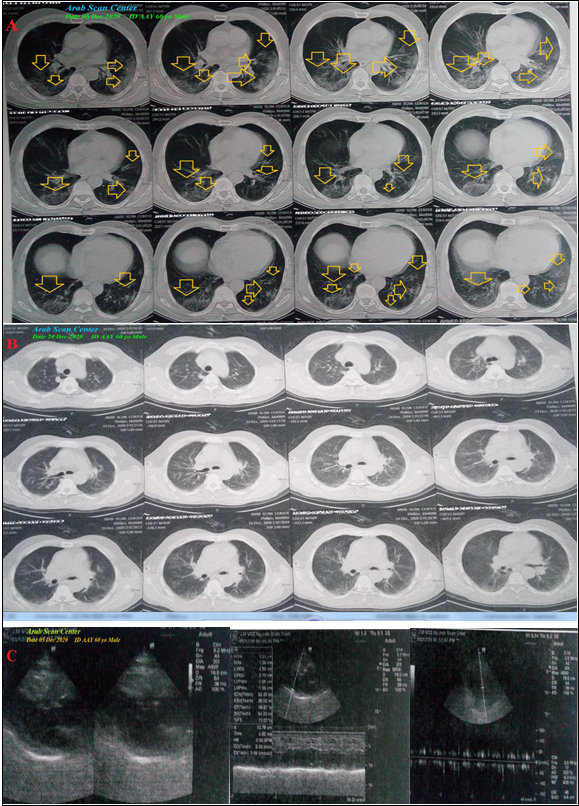
triple sign of hypocalcaemia or Yasser’s sign-in V1-3 leads (Figure 1A). Figure 1: Serial ECG tracings. Figure 2: A: Chest CT scan was done on presentation showing bilateral multiple The patient was tested
for latent tetany which was positive. The initial Complete Blood Count (CBC);
Hb was 14.2 g/dl, RBCs; 4.83*103/mm3, WBCs; 5.29*103/mm3
(Neutrophils; 76%, Lymphocytes: 20%, Monocytes; 3%, Eosinophils; 1% and
Basophils 0%), Platelets; 142*103/mm3. S. Ferritin was high; 547
ng/ml. D-dimer was high (563 ng/ml). CRP was high; 48 g/dl. LDH was high; 776
U/L. SGPT was normal; 25 U/L, SGOT was normal; 42 U/L. Serum creatinine showed
mild elevation; 1.5 mg/dl and blood urea; showed mild elevation; 110.7 mg/dl
was high. RBS was; 91 mg/dl. Ionized calcium was mildly low; 0.71 mmol/L. The troponin test was
positive. After 21 days of management; RBS was normal; 119 mg/dl. CBC; Hb was
12.7 g/dl, RBCs; 4.29*103/mm3, WBCs; 5.84*103/mm3
(Neutrophils: 68%, Lymphocytes: 25%, Monocytes: 6%, Eosinophils: 1% and
Basophils: 0%), Platelets: 85*103/mm3. Serum ferritin was normal;
291 ng/ml. D-dimer was normal (100 ng/ml), CRP was negative (0.4 g/dl), LDH was
still high; 624.94 U/L. SGPT was normal; 19 U/L, SGOT was normal; 37 U/L. Serum
creatinine; 1.3 mg/dl and blood urea; 49.4 mg/dl were normal. Ionized calcium
was normal; 1.23 mmol/L. The troponin test had become negative. The first chest
CT scan was done on presentation showing bilateral multiple patchy ground-glass
pulmonary consolidations (Figure 2A).
Serial ECG tracings were done. ECG tracing was taken within 13 days of
treatment showing down-sloping ST-segment depressions in inferior leads (II,
III, and aVF), in anterior leads (V3-6 leads), with normal sinus rhythm (of VR
of 98). There are also peaked
P-wave in lead II and biphasic in V1 lead (Figure
1B). ECG tracing was taken within 20 days of treatment showing down-sloping
ST-segment depressions in inferior leads (II, III, and aVF), in anterior leads
(V3-6 leads) ± V6 (missed lead), and straight ST-segment depressions in V3 lead
with normal sinus rhythm (of VR of 94). There are also still peaked P-wave in
lead II and biphasic in V1 lead (Figure
1C). An oral nitroglycerine capsule (2.5 mg, twice daily) was added. The
last chest CT scan was done within 20 days of the presentation showing nearly
dramatic improvement of the above ground-glass consolidations (Figure 2B). Echocardiography showed no
detected abnormality with an EF of 58% (Figure
2C). COVID-19 pneumonia with coronary artery spasm and the Wavy triple an
electrocardiographic sign (Yasser Sign) was the most probable diagnosis. ECG tracing was taken
within 35 days of treatment showing normalization of above ST-segment
depressions with normal sinus rhythm of VR 98. There are also still peaked
P-wave in lead II and biphasic in V1 lead. (Figure 1D). Within 24 days of the above management, the patient
finally showed nearly complete clinical, radiological, and laboratory
improvement. The patient was continued on aspirin tablet (75 mg, once daily),
oral nitroglycerine capsule (2.5 mg, twice daily) and diltiazem tablet (60 mg,
once daily), oral calcium, and vitamin-D preparation for 30 days with further
recommended cardiac and chest follow up. Overview:
An elderly farmer male COVID-19 patient presented to physician outpatient
clinic with bilateral pneumonia, AF, evidence of coronary artery spasm, and
Wavy triple an electrocardiographic (ECG) sign or Yasser Sign of hypocalcemia. The objective primary
for my case study was the presence of COVID-19 pneumonia, AF, evidence of
coronary artery spasm, and Wavy triple an ECG sign (Yasser Sign) of
hypocalcemia in POC. The secondary objective
for my case study was the question of; How did you manage the case? I can’t compare the
current case with similar conditions. There are no similar or known cases with
the same management for near comparison. The only limitation of
the current study was the unavailability of the invasive test for coronary
artery spasm. Yasser
Mohammed Hassanain Elsayed, Critical Care Unit, Fraskour Central Hospital,
Damietta Health Affairs, Egyptian Ministry of Health (MOH), Damietta, Egypt,
Email: dryaser24@yahoo.com Elsayed Y.M.H. COVID-19 pneumonia with atrial
fibrillation, coronary spasm, and wavy triple sign (Yasser’s sign); dramatic
reversal at home management (2021) Clinical Cardiol Cardiovascular Med 4: 20-23. COVID-19, Coronavirus, Bilateral pneumonia,
Atrial fibrillation, Wavy triple electrocardiographic sign, Movable-weaning
phenomenon.COVID-19 Pneumonia with Atrial Fibrillation, Coronary Spasm, and Wavy Triple Sign (Yassers Sign); Dramatic Reversal at Home Management
Abstract
Rationale: A novel COVID-19
with a severe acute respiratory syndrome or pneumonia had arisen in Wuhan,
China in December 2019. Emerging atrial fibrillation in COVID-19 patients is
highly significant in cardiovascular medicine. A newly coronary artery spasm in
the presentation of COVID-19 infection has certainly a risk impact on both
morbidity and mortality of COVID-19 patients. Wavy triple an
electrocardiographic sign (Yasser Sign) is an innovated sign of hypocalcaemia
linked to tachypnea and acute respiratory distress.
Patient concerns: An elderly male
COVID-19 patient presented to physician outpatient clinic with bilateral
pneumonia, atrial fibrillation, evidence of coronary artery spasm, and Wavy
triple an electrocardiographic sign (Yasser Sign).
Diagnosis: COVID-19 pneumonia with
coronary artery spasm and the Wavy triple an electrocardiographic sign (Yasser
Sign).
Interventions: Chest CT scan,
electrocardiography, oxygenation, and echocardiography.
Outcomes: Gradual dramatic clinical,
electrocardiographic, and radiological improvement had happened.
Lessons: The reversal of
electrocardiographic ST-segment depressions in a COVID-19 patient after adding
oral nitroglycerine is an indicator for the presence of coronary artery spasm.
It signifies the role of the anti-infective drugs, anticoagulants, antiplatelet,
and steroids in COVID-19 patients with bilateral pneumonia, AF, coronary artery
spasm are effective therapies. The disappearance of AF after initial therapy
may a guide for a good prognosis in this case study. The evanescence of Wavy
triple ECG sign as a hallmark for the existence of the Movable-weaning
phenomenon of hypocalcaemia is recommended for further wide-study.
Full-Text
Introduction
Case
Presentation
Discussion
Conclusion
and Recommendations
References
*Corresponding author:
Citation:
Keywords