Research Article :
Safaa ELMeneza, Rana Fouad and Iman El Bagoury Background: Early-onset sepsis is one of the main causes for
admission of newborns to the neonatal intensive care unit. Traditional markers
are inadequate for identification of early-onset sepsis. Pancreatic stone
protein is a promising sepsis marker in adults with limited studies in neonatal
population. The aim of this study was to assess value of pancreatic stone
protein as a novel sepsis biomarker in diagnosis of early onset neonatal sepsis
in neonates. Neonatal sepsis is a common,
devastating, and overwhelming disease that contributes to morbidity and death.
It has life-long impact plagued by a lack of accurate diagnostic and prognostic
testing
[1]. The clinical signs are non-specific and indistinguishable from those
caused by a diversity of neonatal noninfectious disorders. Early detection and
diagnosis of neonatal sepsis is difficult but extremely important because
prompt institution of antimicrobial
therapy
improves outcomes. Early-Onset
Sepsis
(EOS) is one of the major reasons for the neonatal admission in Neonatal
Intensive Care Unit
(NICU). EOS has been variably defined based on the age at onset, with bacteremia
or bacterial meningitis occurring during 72 hours in infants hospitalized in
the NICU [2]. Neonatal early-onest sepsis occurs in the following criteria
newborns with early-onset sepsis, 85% present within 24 hours, 5% present at
24-48 hours, and a smaller percentage presents within 48-72 hours. Onset is
most rapid in premature neonates [3]. Although of the constant efforts to
diagnose neonatal sepsis still it persist a perplexing topic for neonatologists
due to multiple factors including the lack of ideal diagnostic markers that fit
both full- term and preterm infants. Pancreatic Stone
Protein
(PSP) is a protein secreted by the pancreas recognized by varied scale of
functions, as adhesion and signaling receptors in homeostasis and innate
immunity, it is vital in inflammatory process and leukocyte and platelet
trafficking. Moreover,
the observation that PSP level rose in response to septic insults in mice and
rats encouraged its clinical evaluation as biomarker of sepsis in various
settings and conditions [4]. PSP has recently emerged as a promising sepsis
marker in adults, with high PSP levels predicting sepsis, sepsis associated
multiple-organ failure, in patients with ventilator-associated pneumonia,
post-traumatic sepsis and mortality. Few consistent data are available for PSP
in the clinical setting of neonatal sepsis [5-7]. Our
research question was can Pancreatic stone protein be used as novel marker for
diagnosis of early onset sepsis in neonatal population? The
objective of this study was to assess the value of PSP as a novel sepsis
biomarker in diagnosis of early onset neonatal sepsis. This
study was a case-control study. It was conducted in the NICU of Al-Zahraa
University Hospital. The study included 90 newborn infants, who were allocated
into 2 groups, group 1 with EOS (n=60) and group 2 control, apparently healthy
newborn infants with no risk factors or clinical
manifestations
of sepsis (n=30). Inclusion criteria for the study group were diagnosis of
early onset sepsis in the first 72 hours after birth, with the “presence of at
least two clinical symptoms and at least two laboratory signs in presence of or
as a result of suspected or proven infection (positive culture, or microscopy
polymerase chain reaction)” as suggested by report on the expert meeting on
neonatal and pediatric sepsis 2010 [8].
Diagnosis of cases with negative blood culture was based upon the clinical
sepsis and hematological scores. In
this study full term infants were those >37 weeks of gestation and preterm
infants (32-34) weeks. Exclusion criteria included newborn infants with
congenital anomalies, chromosomal abnormalities or inborn errors of metabolism,
confirmed intrauterine viral infection, perinatal asphyxia. Neonates receiving
parenteral antibiotic at the time of sepsis evaluation or newborn had just
undergone surgery. All
neonates were subjected to history taking, clinical examination, laboratory
investigations including: Complete Blood
Count
(CBC), liver and kidney function tests, blood culture, C-Reactive
Protein
(CRP), and serum pancreatic stone protein using Enzyme-Linked Immunosorbent
Assay (ELISA), kits from Kono Biotech Co.,Ltd, catalogue number: KN 2065Hu (My
Biosource/MBS285689, San Diego, California, USA). Clinical sepsis score
according to Töllner score was done, as well as the hematological score [9,10].
Samples were collected at the time of diagnosis of sepsis. The study was
approved by the ethics committee of the scientific research, Faculty of
Medicine for girls, AL-Azhar University. An informed consent was obtained from
the parents or caregivers of each neonate before enrollment in the study. Data
were collected, coded, revised and entered to the statistical package for
social science (IBM SPSS) version 20. The
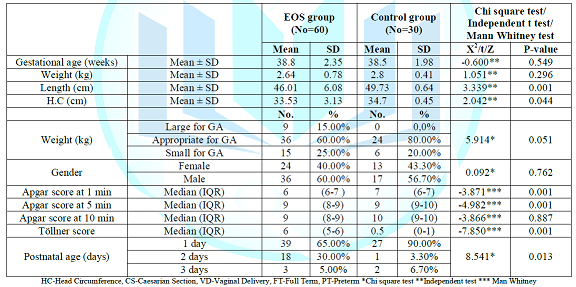
results are shown in Tables 1- 4. Table 1: Clinical characteristics
of the studied newborn infants. PSP
has been studied in adults and shown to accurately predict multi-organ failure
and mortality in patients with ventilator-associated pneumonia and post
traumatic sepsis [5,6]. This study analyzed the role of PSP as a novel sepsis
biomarker in diagnosis of early onset neonatal sepsis in newborn infants. There
was no significant difference in gestational age between EOS group and control
group. There was predominance of male gender (60%) among the sepsis group. The
present study showed significant decrease in Apgar score among sepsis group at
1-5 minutes. Töllner score was higher among sepsis group than the control
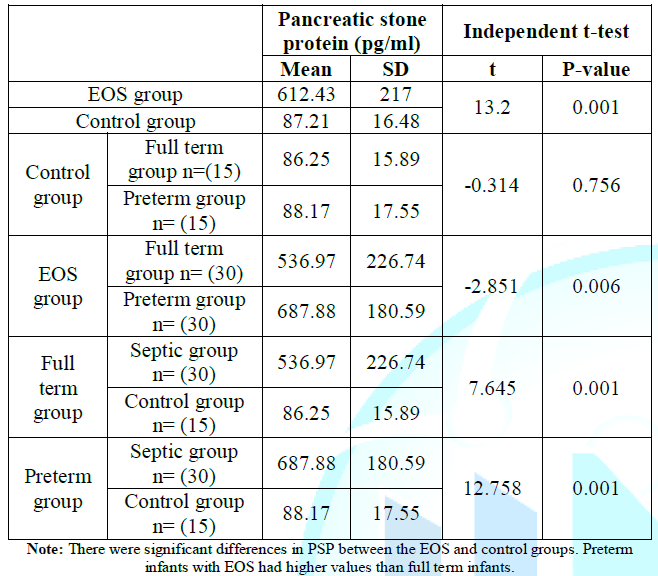
group. The current study results showed the importance of PSP as novel sepsis
marker in diagnosis of early onset neonatal sepsis as well as its prognostic
values. The mean values PSP was increased statistically in ESO group in
comparison to control group (P=<0.001). This increase among the sepsis group
may be due to promoting cellular proliferative responses in the pancreas by PSP
and activation of polymorph nuclear cells, PSP/reg binds and activates
neutrophils behaving as an acute-phase protein that responds to injury during
the early phase of infection [5]. Animal
studies have shown induction of PSP expression in subset of intestinal and
gastric cells by stress conditions in absence of direct pancreatic
inflammation
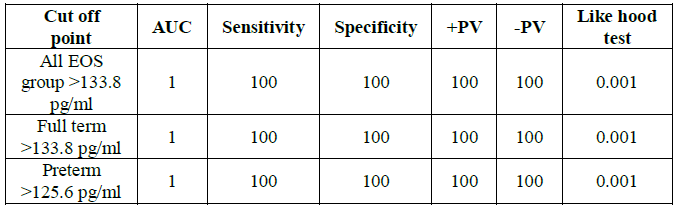
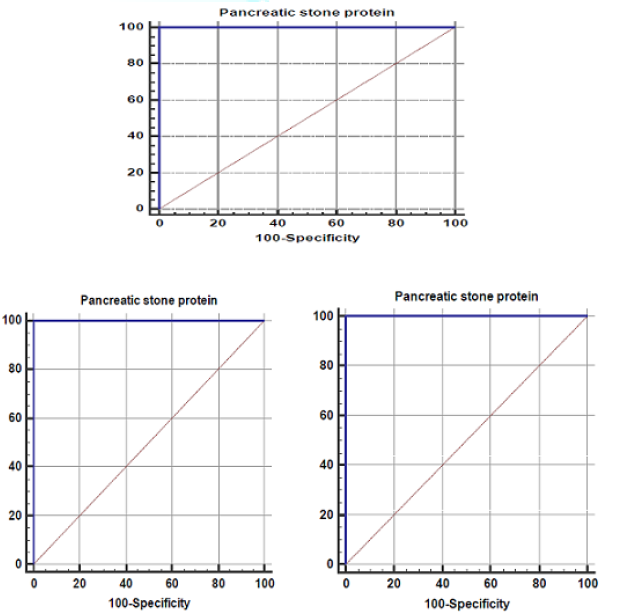
[8,11]. In this study, PSP at a cutoff value of
>133.8 pg/ml, had the sensitivity, specificity, Positive
Predictive Values (PPV) and Negative Predictive
Values (NPV) of 100%, and the Area
Under Curve (AUC) was 1.000 (𝑝 <
0.001) for the EOS group, this results are more or less the same as those of
Rass et al. who reported that at a cutoff level of 12.96 mg/mL, the sensitivity
was 96.2%, the specificity was 88.5%, PPV value was 95.8%, NPV was 89.3%, and
AUC was 0.87 and to Schlapbach, et al. who reported that PSP has high NPV of
90% and 79% sensitivity in newborn infants, also to results by Wu, et al. who
reported sensitivity of 79.7% in pediatrics patient. Also Dima, et al. found
that the diagnostic performance of PSP was superior to that of traditional
markers [7,12-14]. Further analysis of the data for the preterm infants (32-34)
weeks, showed 100% sensitivity, specificity as well as PPV and NPP at a cut off
value of >125.6 pg/ml. Table 2: Pancreatic stone
proteins in the studied groups. Table 3: Pancreatic stone
proteins and neonatal outcome. There
was significant increase in PSP mean values in preterm infants with EOS in
comparison to full term infants (P=0.006). It could be due to systemic
exaggerated immature inflammatory response to invasive bacteria and significant
stress among the studied preterm infants. Schlapbach, et
al. reported that PSP has bell-shaped distribution from birth to adulthood in
normal population, this is opposite to the results of current study [15]. On
the other hand, Stoll et al. stated that the risk of early onset sepsis
increases with decrease of gestational age because of the inability of white
blood cells to carry out phagocytosis, immaturity of
the immune system, low complement levels, and hypogammaglobulinemia [16]. As far as
we know this study was first to look at PSP in full term and preterm infants.
To understand the exact mechanism, it may need further larger study. In
practice, different thresholds for PSP may be needed to detect severity of
illness in newborns compared to older age groups. So this study looked also at
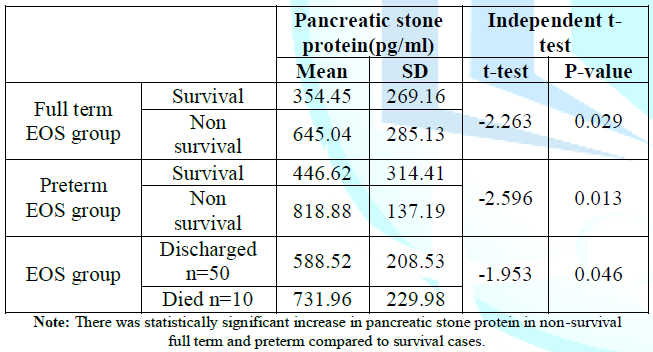
the differences of PSP between the survival and non-survival cases. There was
statistically significant increase in PSP in non-survival EOS group weather
preterm or full term than those survival cases of EOS group (P=0.046). The increase
in PSP could be due to additional stress and severity of inflammation among
severely sick dead cases that led to expression of more PSP, also metabolic
disturbances and respiratory failure lead to acidosis, which can increase
expression of PSP [15]. Previous
studies showed significant PSP increase in presence of significant stress and
multi-organ dysfunction syndrome in critically ill children and patients who
died [17]. These findings agree with those of Que, et al. who found that risk
of mortality in adult population increased continuously for each ascending
quartile of PSP in a prospective cohort of patients with sepsis requiring (Intensive
care unit) ICU management [18]. In
the current study, there was no significant correlation between CRP and PSP in
EOS group. In earlier study we showed that CRP had initial low sensitivity 75%,
specificity 33%, PPV 83% and NPV 24%, during the early phases of infection,
hence it is unhelpful in the initial diagnosis of EOS [19]. Serial
determinations improve the diagnostic accuracy and are useful for evaluating
the response to treatment. CRP considered as a “specific” but “late” marker of neonatal
infection.
The best predictive ability of CRP for EOS lies when it is measured within 24-48
hours of birth or a rising CRP level is seen [20]. These
results attach with those of Schlapbach, et al. who revealed that the
performance of PSP was comparable or superior to other markers such as CRP, PCT
or soluble Human Triggering Receptor Expressed on Myeloid Cells-1 (sTREM-1),
suggesting PSP is independently increased in presence of infections. The PSP is
a rapid laboratory test (<1.3h) and require minimal blood volume (<50 𝜇L)
[7]. PSP is more sensitive, specific and has a good negative predictive value
compared to CRP confirming its value as marker to rule out early onset neonatal
sepsis. In
the present study PSP did not increase from postnatal age day 1 to day 3 in the
EOS groups (P=0.806), Schlapbach, et al. observed a slow increase in PSP
concentrations over the first days of life [15]. Also there was no significant
difference in mean values of PSP in relation to gender in the studied groups. This
study showed significant correlation of PSP with clinical Töllner score and
hematological score. This may strengthen the rule of clinical sepsis score and
hematological score in diagnosis of sepsis in limited resources countries. PSP
can safely guide the decision to initiate empirical antibiotic treatment in
infants with suspected EOS. Errors related to use of anti-infective drugs was
reported in 83.4% of a study done by ELMeneza, et al [21]. Finally, the present
study revealed that PSP is valuable in both diagnosis and prognosis of neonatal
sepsis. The
limitations of this study include the relatively small sample size resulting
inability to explain the significant increase of PSP in preterm infants than
full term infants with EOS. In conclusion, our findings advocate that role of
PSP as a valuable marker in diagnosis of neonatal EOS. PSP has high sensitivity
and specificity, it may empower the neonatologist for safe care and judicious
use of antibiotic. PSP may assist in distinguishing the serious cases that may
have bad prognosis. Recommendation PSP
can be used as a new marker for diagnosis of early onset sepsis. Further study should
be conducted with larger number of neonates to confirm PSP values in early
diagnosis and prognosis of neonatal sepsis especially among preterm and very
low birth weight infants. Statement
of Ethics The
parents have given their informed consent and the study protocol was approved
by the Faculty of Medicine for Girls ethical committee. 1.
James
L Wynn. Defining neonatal sepsis (2016) Curr Opin Pediatr 28: 135-140. 2.
Edwards
MS. Postnatal infections. In: Neonatal-Perinatal Medicine, Fanaroff and Martins
(Eds) (2012) Mosby Elsevier, USA 791-804. 3.
Klinger
G, Levy I, Sirota L, BoykoV, Reichman B, et al. Epidemiology and risk factors
for early onset sepsis among very-low-birthweight infants (2009) Am J Obstet
Gynecol 201: 38.e1-38.e6. https://doi.org/10.1016/j.ajog.2009.03.006 4.
Philippe
E, Yok-Ai Q and Fabien R. Measurement of pancreatic stone protein in the
identification and management of sepsis (2019) Biomark Med 13: 135-145. https://doi.org/10.2217/bmm-2018-0194 5.
Keel
M, Harter L, Reding T, Sun L, Hersberger M, et al. Pancreatic stone protein is
highly increased during posttraumatic sepsis and activates neutrophil
granulocytes (2009) Critical Care Medicine 37: 1642-1648. https://doi.org/10.1097/ccm.0b013e31819da7d6 6.
Boeck
L, Graf R, Eggimann P, Pargger H, Raptis D, et al. Pancreatic stone protein: a
marker of organ failure and outcome in ventilator-associated pneumonia (2011)
Chest 140: 925-932. https://doi.org/10.1378/chest.11-0018 7.
Schlapbach
LJ, Graf R, Woerner A, Fontana M, Zimmermann-B U, et al. Pancreatic stone
protein as a novel marker for neonatal sepsis (2013) Intensive Care Medicine
39: 754-763. https://doi.org/10.1007/s00134-012-2798-3 8.
Rossi
P and Botgros R. Report on the Expert Meeting on Neonatal and Paediatric Sepsis
(2010) European Medicine Agency, UK. 9.
Töllner
U. Clinical studies and sepsis score (1982) European J Pediatrics 138: 331-337.
10.
Pramana
KP, Kardana M and Putu GA. Diagnosis Accuracy of Hematological Scoring System
in Early Identification of Neonatal Sepsis (2016) Bali Med J 5: 139-144. https://doi.org/10.15562/bmj.v5i3.310 11.
Graf
R, Schiesser M, Reding T, Appenzeller P, Sun LK, et al. Exocrine meets
endocrine: pancreatic stone protein and regenerating protein-two sides of the same
coin (2006) J Surg Res 133: 113-120. https://doi.org/10.1016/j.jss.2005.09.030 12.
Rass
AA, Talat MA, Arafa MA, Mohamed
A, Anwar A, et al. The role of pancreatic stone protein in diagnosis of early
onset neonatal sepsis (2016) BioMed Res Int 2016: 1-8. https://doi.org/10.1155/2016/1035856 13.
Wu
R, Zha L, Hu JH, Wu JM and Tian ZF. The value of pancreatic stone protein in
the prediction of infected neonates (2017) Minerva Pediatr 69: 489-494. 14.
Dima
M, Iacob D, Marginean O and Iacob ER. New emerging biological markers of
neonatal sepsis (2017) J Res Med Sci 22: 65. https://doi.org/10.4103/jrms.jrms_912_15 15.
Schlapbach
LJ, Giannoni E, Wellmann S, Stocker M, Ammann RA, et al. Normal values for
pancreatic stone protein in different age groups (2015) BMC Anesthesiology 15: 168.
https://doi.org/10.1186/s12871-015-0149-y 16.
Stoll
BJ, Hansen NI, Sánchez PJ, Faix RG, Poindexter BB, et al. National institute of
child health and human development neonatal research network early onset neonatal
sepsis: the burden of group B streptococcal and E. coli disease continues (2011)
Pediatrics 127: 817-826. https://doi.org/10.1542/peds.2010-2217 17.
Jiri
Z, Kyr M, Vavrina M and Fedora M. Pancreatic stone protein-a possible biomarker
of multiorgan failure and mortality in children sepsis (2014) Cytokine 66: 106-111.
https://doi.org/10.1016/j.cyto.2014.01.009 18.
Que
YA, Delodder F, Guessous I, Graf R, Bain M, et al. Pancreatic stone protein as
an early biomarker predicting mortality in a prospective cohort of patients
with sepsis requiring ICU management (2012) Critical Care 16: R114. https://doi.org/10.1186/cc11406 19.
ELMeneza
SA, Esmail HO, Elbagoury EM and Abd Allah NA. Soluble triggering receptors
expressed on myeloid cell-1 and proadrenomedullin for diagnosis and prognosis
of early onset neonatal sepsis (2018) EC Paediatrics 7: 619-628. 20.
Hofer
N, Zacharias E, Müller W and Resch B. An update on the use of C-reactive
protein in early-onset neonatal sepsis: current insights and new tasks (2012)
Neonatology 102: 25-36. https://doi.org/10.1159/000336629 21.
EL
Meneza S, Habib A and Abd ElSalam RM. Analysis and identifying risk profile for
medication errors in the neonatal intensive care units (2018) EC Paediatrics 7:
669-684. Safaa ELMeneza, Pediatrics department, Faculty of
Medicine for Girls, AL-Azhar University, Egypt, Email: safaa5@hotmail.comPancreatic Stone Protein as a Novel Marker for Early Onset Neonatal Sepsis
Abstract
Methods: This was case control study with 90 newborn infants
were involved. They were admitted to Al-Zahraa University hospital with
diagnosis of early-onset sepsis. The cases were allocated into 2 groups, group
(1) the early-onset sepsis group and group (2) control group of normal newborn
infants who had no sepsis.
Results: Pancreatic stone protein was significantly higher
in early-onset sepsis group than control group with 100% sensitivity,
specificity, positive predictive value, negative predictive value at cut off
point>133.8 pg/ml and cut off value of 125.6 pg/ml for preterm infant. There
was statistically significant increase of Pancreatic stone protein among
non-survival cases. There was correlation between Pancreatic stone protein and
weight, I/T ratio, Immature myeloid series, Pco2, bicarbonate, urea, Töllner
score and haematological score.
Conclusions:
Our findings advocate that role of Pancreatic stone protein as a valuable
marker in diagnosis of neonatal early-onset sepsis. Pancreatic stone protein
has high sensitivity and specificity, it may empower the neonatologist for safe
care and judicious use of antibiotic. Pancreatic stone protein may assist in
distinguishing the serious cases that may have bad prognosis. Full-Text
Introduction
Objective
Patient and
Methods
Study
design
Procedure
Statistical analysis
Results
Discussion
References
*Corresponding author
Citation
ELMeneza S, Fouad R and El Bagoury I. Pancreatic stone protein as a novel marker for early onset neonatal sepsis (2019) Edelweiss Pediatrics J 1: 1-4
Early neonatal period, Neonatal sepsis, Newborn infant, Preterm, Neonatal Outcome, Pancreatic Stone Protein, Sepsis.