Case Report :
Miki Kashiwagi, Takahiro Abe,
Yuske Komiyama, Noriko Komatsu, Shoko Tateishi and Kazuto Hoshi Some patients with Rheumatoid Arthritis suffer with
Temporomandibular Disorders (TMD). A 36-year-old Asian female presented to our
hospital with Temporomandibular Joint (TMJ) symptoms, including pain. The
maximum self-opening distance was 23 mm at first visit. As symptoms were worse
in the morning and also started occurring in other joints, rheumatologists were
consulted. The rheumatologists prescribed Etanercept (ETN), a tumor necrosis
factor inhibitor which is commonly used in the early stages of Rheumatoid Arthritis (RA). The use of
ETN together with conservative therapy for the TMJ improved the symptoms in the
affected joints. No therapy for TMJ symptoms in RA patients has yet been
established. However, the findings of this case suggest that the usage of
biological products from the early stage of RA and jaw-training may be possible
to manage TMJ symptoms. The
incidence of Rheumatoid Arthritis (RA) is 0.5-1% of the global population [1].
According to the Ministry of Health, Labor and Welfare, an estimated
700,000-800,000 people in Japan suffer from RA. It is three times more common
in women than men, and usually develops between the ages of 30 to 50. The life
expectancy of patients with RA is 20% lower than that of the general
population. RA is a progressive condition, where inflammation causes joint
destruction and synovial proliferation (pannus) around the articular cartilage.
Symptoms include pain, tenderness, swelling and morning stiffness, often in the
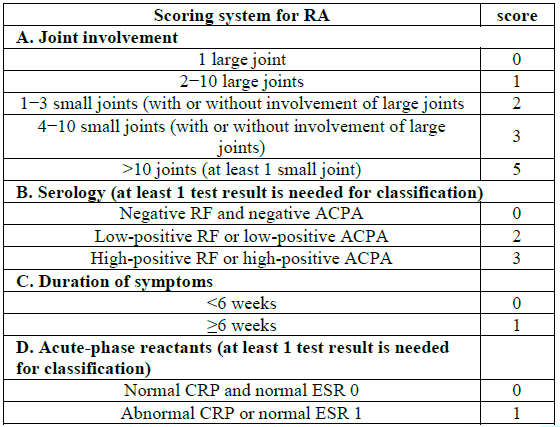
small joints of the hands and feet. In 2010, the European League Against
Rheumatism (EULAR) published new classification criteria for RA [2]. Table 1
shows the different areas that are evaluated and scored. When the total score
is 6 or higher, the patient is diagnosed with RA. Early
diagnosis and medical treatment helps to prevent joint destruction. For the
management, Methotrexate (MTX), anti-rheumatic drugs, including
Disease-Modifying Anti-Rheumatic Drugs (DMARDs), and biological products such
as Tumor Necrosis Factor inhibitors (TNF) or humanized anti-IL-6 receptor
antibodies are all used. Among RA patients, some have TMJ symptoms.
Bessa-Nogueira, et al. [3] reported that 70% of patients with RA had some TMJ
symptoms, while Trenwith and Beale [4] noted that 62% of RA patients complained
of TMJ symptoms at least once. Condylar volume and ramus height get smaller in
Juvenile Idiopathic Arthritis (JIA) patients, which is one of the rheumatic
disease in childhood [5]. At the moment, TMJ symptoms of RA patients seems to
be little agreement as to how to manage in such cases (Table 1). A
36-year-old Asian female presented to the university of Tokyo hospital with
pain in the left TMJ. She had been aware of sound produced by the left TMJ from
around the age of 11, but had not experienced any pain or restricted opening.
She became aware of the pain in the left TMJ one year before she first presented,
and it had become sustained one month before presenting. The pain was worse in
the morning and was less intense in the evening. Her past medical history
included insomnia, pyelonephritis and infertility. Physical examination
revealed multiple findings. There was facial asymmetry of the face (Figure1A). Figure
1A: Facial photo with mouth closed (left) and
opened (right). The
maximum self-opening distance of the mouth was 23 mm, and the forced-opening
distance was 28 mm. Misalignment of the mandible was seen on the left side when
opening. Pain and tenderness were experienced during movement of the left
joint. Crepitus was observed in the left TMJ. Redness of the oral mucosa and
gingiva was noted, but there was no swelling (Figure 1B). Figure
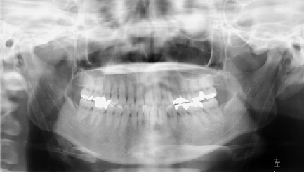
1B: Oral photos at first visit. Orthopantomography
showed no deformity of the mandibular condyle. MRI revealed a joint disc
derangement without reduction of the left TMJ. On the basis of these findings,
a primary diagnosis of TMJ arthralgia and joint disc derangement without
reduction was made. Treatment of these TMD was with an Oral Appliance (OA) and
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs). We used stabilization appliance
for reducing TMJ pain. Further symptoms were reported soon after the TMJ
symptoms had begun (Figure 2A, 2B). Figure
2A: Orthopantomography at first visit. Figure
2B: Orbito-ramus projection at first visit. The
right shoulder became difficult to abduct. Moreover, pain in the
Metacarpophalangeal (MP) joint of the second finger in the left hand appeared.
Pain and swelling in the left third finger MP joint and pain in both feet thumb
also appeared. At this time point, we consulted the allergy and rheumatology
team, and a second diagnosis of RA was made. Using the new classification
system for the diagnosis of RA, the swelling and pain of 4 joints was counted
as 3 points, anti-cyclic citrullinated peptide antibody was 19.5 HU/ml and was
counted as 3 points, and symptoms over 6 months was counted as 1 point. The
total score was more than 6 points, which confirmed a diagnosis of RA. By the
rheumatology team, she was started drug therapy for RA. Salazosulfapyridine
(SASP), ETN and Prednisolone (PSL) were selected in order. SASP is a DMARD
which is used globally in the treatment of RA [6]. ETN, a biological product,
is also used to treat RA [7]. PSL is synthetic adrenocortical hormone which
works as anti-inflammatory agent. Therapeutic efficacy was evaluated using
X-ray, MRI, blood tests, DAS 28-CRP and by checking mouth-opening distance. The
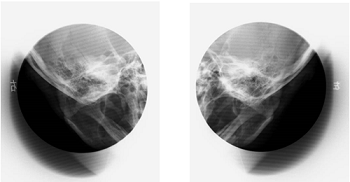
panoramic TMJ radiograph showed osteophysis, flattening, and osteosclerosis
around the erosion of the left mandibular condyle (Figure 3). Figure
3: Panoramic TMJ radiograph at 0 days, 6 and
33 months after initial presentation. In
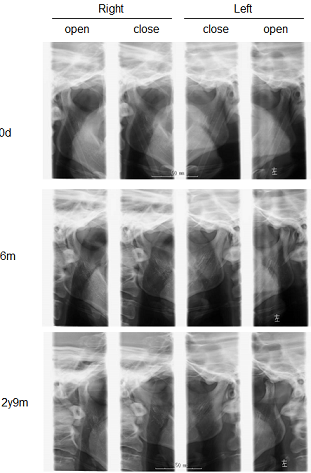
the T2-weighted MRI image, a low signal area (bone edema) was detected under
the cortex of the left anterior mandibular condyle, indicating a progressing
osteosclerosis. In the Proton-Density Fast Spin-Echo (PD FSE) image, the left
anterior derangement of the joint disc was preceded, and the left mandibular
cortical bone became thinner and there was progression of osteophytosis after 3
years. In the right TMJ, there was no change in TMJ disc derangement with
reduction and no significant change in the condyle (Figure 4). Figure
4: MRI of the right and left temporomandibular
joints at 9, 18, and 33 months. Blood
tests were done to check for certain markers of RA such as Rheumatoid Factor
(RF), Hemolytic Complement Activity (HCA) (CH50), Matrix Metalloproteinase 3
(MMP-3), Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP).
During treatment with SASP and ETN, CH50 was within the normal range. RF was
within the normal range while ETN was used. MMP-3 was high, but values
decreased while treatment with ETN continued. ESR was high before ETN
administration and during ETN discontinuation. She needed to discontinue the
ETN because of pregnancy, as a result, causing the concentrations of RA markers
to increase. MMP-3 might be raised by PSL. DAS 28-CRP was 3.01 at 2 months,
1.73 at 11 months, 1.27 at 12 months, 3.14 at 31 months, and after the first
visit (Figure 5). When
ETN was started, the DAS 28-CRP value decreased. The mouth-opening distance
increased after the start of ETN administration. Even after discontinuation,
the patient was able to maintain the opening distance to some extent because
she continued visiting the hospital and doing jaw-training. Numeric rating
scale (NRS) was showed low score during ETN administration (Figure 6,7A,7B). Figure
7B: Oral photos at 2
years. Newly
revised RA classification criteria by the EULAR in 2010 increased the
diagnostic sensitivity in the early stages of RA. With the increase in the
number of patients diagnosed as having RA due to the less strict diagnostic
criteria, the number of patients with RA in the TMJ is expected to increase.
According to a report by Tabeling, et al. [8], the TMJ is affected in
approximately 50% of cases of RA. In addition, as mentioned above, it was
reported that some temporomandibular joint symptoms were found in 70% of RA
patients [3]. Further,
Marini, et al. [9] reported that erosive changes in the TMJ were detected on
X-ray in two-thirds of patients. In this case, fortunately we were able to
diagnose the patient as having RA early in the disease course by focusing on
the findings that the initial symptom developed in the TMJ, that joint symptoms
also developed in the hands and feet, and that these symptoms were worse in the
morning, among others. In cooperation with rheumatologists in our hospital, the
patient was treated with ETN early and were able to alleviate symptoms in
joints of the whole body, including the TMJ. The present case suggests the
effectiveness of a biological product (ETN, a TNFα inhibitor) in controlling RA
of the TMJ in its early stage, and confirmed the necessity of continuous
treatment. Etanercept (ETN) is a glycoprotein consisting of the Fc region of
human IgG1 and the 75-kDa human tumor necrosis factor receptor 2. It exerts an
anti-rheumatic and anti-inflammatory action through a mechanism in which the
human TNF soluble receptor region works as a decoy to capture excessively
produced TNFα and TNFβ and inhibits their binding to receptors on the cell
surface. After the treatment of the ETN, the patient became pregnant and gave
birth, therefore, necessitated to stop the ETN treatment during this time.
After that, DAS28-CRP score was elevated, demonstrating a relapse of disease
activity. Blood tests also showed increasing the levels of RF, MMP-3, CH50 and
ESR. Exacerbation
of some TMJ symptoms, such as increased pain, were also observed accompanied
with the increased systemic disease activity. In contrast, the alleviation of
TMJ symptoms was achieved when the ETN treatment was resumed. Recently, usage
of biological products for RA has increased, and many papers have reported
their strong therapeutic effect. For example in oral diseases, ETN improves
periodontal conditions by reducing periodontal inflammation. However, there are
only a few papers on the use of biological products for TMJ symptoms. It has
been suggested that biological products can be effective for temporomandibular
joint symptoms as well as joints in the whole body, although this requires
confirmation in a larger number of patients [10-12]. Considering the
mouth-opening distance, an indicator of TMJ dysfunction, the combination of
jaw-training and using OA are thought to have been effective. Generally,
exercise therapy at the initial stage of RA is important to prevent loss of normal
function in joints due to the rapid onset of deterioration. Similarly, we think
that mouth-opening distance was maintained by the jaw-training and that the use
of OA stabilized occlusion helped to alleviate the pain by reducing external
forces on the joint surfaces. Moreover, with the treatment of ETN, the TMJs
became stabilized by inhibiting inflammation. No therapy for TMJ symptoms in RA
patients has yet been established. In our experience of one case, there is
little evidence; however, we believe that the usage of biological products and
jaw-training with an OA may be effective for RA with TMD. In the future,
further consideration including many cases will be needed. Informed
consent was gained for inclusion of a de-identified photograph. 1. Silman
AJ and Pearson JE. Epidemiology and genetics of rheumatoid arthritis (2002)
Arthritis Res 4: S265-S272. https://doi.org/10.1186/ar578 2. Aletaha
D, Neogi T, Silman AJ, Funovits J, Felson DT, et al. 2010 rheumatoid arthritis
classification criteria: an American college of rheumatology/European league
against rheumatism collaborative initiative (2010) Arthritis Rheum 69: 2569-2581. https://doi.org/10.1002/art.27584 3. Bessa-Nogueira
RV, Vasconcelos BC, Duarte AP, Goes PS and Bezerra TP. Targeted assessment of
the temporomandibular joint in patients with rheumatoid arthritis (2008) J Oral
Maxillofacial Surgery 66: 1804-1811. https://doi.org/10.1016/j.joms.2007.08.037 4. Trenwith
JA and Beale G. Rheumatoid arthritis in the temporomandibular joint (1977) N Z
Dent J 73: 195-199. 5. Farronato
M, Cavagnetto D, Abate A, Cressoni P, Fama A, et al. Assessment of condylar
volume and ramus height in JIA patients with unilateral and bilateral TMJ
involvement: retrospective case-control study (2019) Clin oral investigatn 23:
1-9. https://doi.org/10.1007/s00784-019-03122-5 6. Hilliquin
P, Munoz A and Menkes CJ. Salazosulfapyridine in rheumatoid arthritis. A study
of 49 patients (1992) Ann Med Interne 143: 149-154. 7. Haraoui
B and Bykerk V. Etanercept in the treatment of rheumatoid arthritis (2007) Ther
Clin Risk Manag 3: 99-105. https://doi.org/10.2147/tcrm.2007.3.1.99 8. Tabeling
HJ and Dolwick MF. Rheumatoid arthritis: diagnosis and treatment (1985) Florida
Dental J 56: 16-18. 9. Marini
I, Vecchiet F, Spiazzi L and Capurso U. Stomatognathic function in juvenile
rheumatoid arthritis and in developmental open-bite subjects (1999) ASDC J Dent
Child 66: 30-35. 10. Maspero
C, Giannini L, Galbiati G, Prevedello C and Farronato G. Periodontal conditions
in juvenile idiopatic arthritis (2017) Minerva Stomatologica 66: 43-50. 11. Foeldvari
I, Tzaribachev N and Cron RQ. Results of a multinational survey regarding the
diagnosis and treatment of temporomandibular joint involvement in juvenile
idiopathic arthritis (2014) Pediatr Rheumatol Online J 12: 6. https://doi.org/10.1186/1546-0096-12-6 12. Kurtoglu
C, Kurkcu M, Sertdemir Y, Ozbek S and Gurbuz CC. Temporomandibular disorders in
patients with rheumatoid arthritis: A clinical study (2016) Nigerian J Clinical
Practice 19: 715-720. Takahiro Abe, Department of Oral, Maxillofacial
Surgery and Orthodontics, the University of Tokyo Hospital, Tokyo, Japan, Tel:
+81-3-3815-5411, Fax: +81-3-5800-6832, Email: abetakahiro.dream@gmail.com Kashiwagi M, Abe T, Komiyama Y, Komatsu N, Tateishi S, et al. Efficacy of
etanercept with jaw-training for rheumatoid arthritis with firstly
temporomandibular joint symptoms: a case report (2019) Rheumatic dis treatment
J 1: 6-9. Temporomandibular joint, Rheumatoid arthritis,
Biological products, Tnf inhibitor, Etanercept.Efficacy of Etanercept with Jaw - Training for Rheumatoid Arthritis with Firstly Temporomandibular Joint Symptoms: A Case Report
Abstract
Full-Text
Introduction
Case Report



Figure
5: Time series data for blood test markers for
Rheumatoid Arthritis (RA) and drugs used for RA. rheumatoid factor (RF); CH50,
Hemolytic Complement Activity (HCA); Matrix Metalloproteinase 3 (MMP-3);
Erythrocyte Sedimentation Rate (ESR); C-Reactive Protein (CRP);
Salazosulfapyridine (SASP); Etanercept (ETN); Prednisolone (PSL).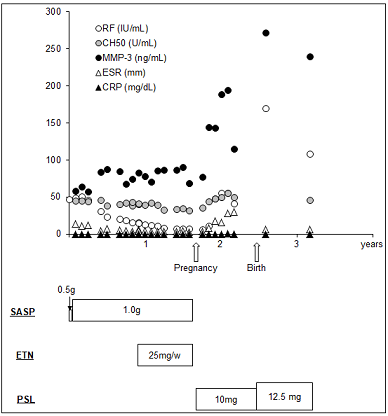
Figure
6: Time series data for mouth-opening
distance, numeric rating scale, temporomandibular disorder treatment and drugs
used for Rheumatoid Arthritis (RA). Numeric Rating Scale (NRS); Oral Appliance
(OA); Salazosulfapyridine (SASP); Etanercept (ETN); prednisolone (PSL).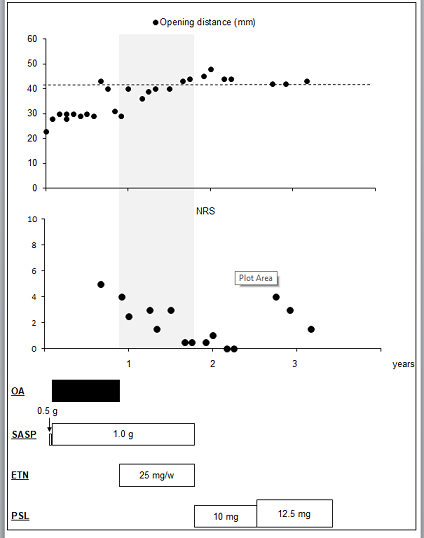
Figure
7A: Facial photo with mouth closed (left) and
opened (right) at 2 years.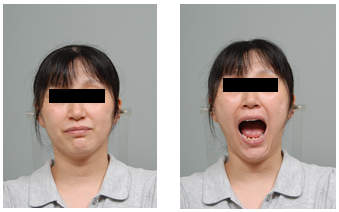

Discussion
Patient
consent
Reference
*Corresponding author
Citation
Keywords