Commentary :
Everyone
agrees that a good understanding of occlusion is essential to ensure optimum
dental health. Unfortunately, that seems to be the only point of consensus for
this important, yet controversial subject. Occlusion is often described as
troublesome, complex, and incoherent, but confusing seems to describe it best. Christensen
comments: Unfortunately, occlusion in its broad
definitions is not a popular subject in CE or in actual practice. Although
occlusion principles permeate almost all of dentistry, the area is confounded
by confusing theories, non-practical techniques, contradictory beliefs, and
practitioners unaware of the basic concepts of occlusion. As a result, most
dental patients go without the benefits of dental therapy based on several occlusal
principles [1]. The
confusion has left us with many unanswered questions, the most important being,
the precise role that occlusion plays in the etiology of Temporo Mandibular Joint Disorders (TMJD). Since it
is unknown, we have to consider the possibility that the way we are doing our
work, may be a contributing factor. The agenda for this commentary is in three
parts. The first part will thoroughly discuss the three factors that have
largely contributed to this abstruseness. The second will be dedicated to Para
function, and the third will review how dental work is being performed today,
and will conclude with guidelines for the restorative dentist that will
minimize and prevent problems with the Temporo Mandibular Joint (TMJ). Three
Sources of Confusion But today, there are two
additional meanings. Dorlands Pocket Medical Dictionary first defined dental
occlusion correctly as‚ the closure of teeth, but later expanded the definition
to the contact of the teeth of both jaws during those excursive movements of
the mandible essential to the function of mastication. [3] Why did they do this
when early studies suggested that; 1. Teeth rarely and lightly touch during mastication [4] and 2. Excursive
movements of the mandible are not essential to the function of mastication? [5] The dental profession had
witnessed patients grinding their teeth in lateral excursions, saw that it was
doing damage, and sought to find the most comfortable pathway, i.e., the
horizontal vector with the least resistance or interference for them to do so.
Many assumed that these horizontal excursions were an integral part of normal
function, when in reality it is parafunction. People do not
normally
eat in horizontal excursions unless forced to do so by a flattened dentition. Still another description over
the years, the word occlusion morphed into a homonym for the stomatognathic
system. Jablonskis definition of occlusion is
a sixty word description of all the components of the stomatognathic system.
[6]. It is not a valid definition of occlusion. The different interpretations
are a major distraction. It clouds the issues and makes questions such as, what
has occlusion got to do with TMD? impossible to answer. Are we asking if tooth
contact during closure is causing a problem with the TMJ, or do we want to know
if the stomatognathic system is not functioning properly? Modern day texts on occlusion do
not just describe the simple touching of upper and lower teeth, but rather
present a detailed analysis of the whole stomatognathic system. Occlusion (the
way teeth touch each other during closure) and the stomatognathic system are
two distinct entities and should be described separately to remove the present
ambiguity. Function
of the Stomatognathic System: Two Different Views The
Vertical Function Paradigm: In this model,
the mandible functions vertically. We talk vertically, we swallow vertically,
and
we eat vertically. The vector of mastication is a vertical teardrop with a
lateral movement of 5mm to 6 mm during the first phase of chewing, and as the
teeth approach each other, the lateral displacement lessens to 3mm to 4mm from
the starting position. The mandible is guided into position during closure by
the occlusal incline planes of the teeth. It is not a consistent and reproducible
movement, but is a function of head position. As
the head tilts forward, the mandible goes forward. After each vertical
function, the mandible returns to a state of physiological rest [7]. During opening and closing, there
is condylar centricity where the axis is maintained, and upon complete closure,
the condyles are seated in the anterior-superior
portion of the glenoid fossae. Border movements
are seldom used and most mandibular movements take place within a reasonably
limited three dimensional space. The model in this paradigm is free from parafunction. The
Horizontal Function Paradigm: While there is
no disagreement that we talk and swallow vertically, the horizontal paradigm is
focused on the premise that the mandible functions laterally, rather than
vertically. How did this come about? In the early 20th century there
were a number of dentists who were preoccupied with the mandibles ability to
rotate around axes in three planes. The study of these jaw movements became
known as gnathology, and its followers gnathologists.
It was the objective of the gnathologists to produce a proper occlusal form
which was dictated by the determinants of mandibular movements, i.e., to create
an occlusal surface that would accommodate free passage for the opposing
dentition. Their goal was to eliminate
interferences in laterotrusive movements from centric. It was called optimal
functional occlusion [8]. But theres a conflict. Functional
occlusion is defined as the touching of upper and
lower teeth during mastication and deglutition-both are vertical not
horizontal. So the gnathologists had the perception that it is normal to
function in lateral excursions, but the reality is that it is parafunction. The gnathologists had another
conflict: the anterior teeth which are a major interference to anterior
excursions. If they were to eliminate that obstacle, they would have to shorten
the incisors considerably. Now what? Their solution was to make lemonade. They
declared that that purpose of the anterior teeth being longer was to disengage
the posterior teeth during these parafunctional
excursions for their protection. It was called anterior
guidance. Nothing was said about the trauma that the anterior teeth would
receive during this exercise. So on the one hand, we have a
paradigm that describes a system that functions vertically, pays little
attention to border movements, and is free from parafunction. On the other, we
have a paradigm whose goal is to eliminate interferences in laterotrusive
movements. Which is best? The vertical paradigm is
the model we want to emulate as it is free from parafunction. If parafunction
does occur, treatment should focus on management and prevention, not on
accommodation. There are three key benchmarks
that are used when evaluating the overall status of the stomatognathic system:
the condyle, the muscles of mastication, and the dentition. There is no
disagreement that when the system is healthy and functioning efficiently, the
muscles of mastication are relaxed and the condyles are seated properly in the
anterior superior part of the fossae. There are however, major questions
regarding the dentition. There is no consensus regarding their morphology, how
exactly they should touch each other in closure, and more importantly, their
involvement in TMJ disorders. From an engineering point of
view, what is the best design for teeth that allows the system to function
efficiently? There are design principles that
appear to govern the structure-function relationship in organisms, i.e., there
is an interface between mechanical engineering and biology. The idea being that
biological
materials and structures are designed for specific functions [9]. In regard to
teeth, the original architect gave us a perfect example. The purpose of the
fossae is to hold food for cutting, while the sharp cusps have two purposes: to
cut the food and to direct mastication forces vertically down the long axis
upon closure. The space between the incline
planes allows resistance-free repositioning of the mandible/condyle not only
during swallowing, but anterior posterior postural changes as well. So it would
appear that the original design or morphology of our teeth is best suited to
serve our stomatognathic system. But unfortunately, this is not the standard
that everyone emulates. For instance, when constructing
removable dentures, we have a choice of seven different designs for the
posterior teeth-from 33 degrees to flat plane occlusion. Now, why would we want
to provide flat plane occlusion for a 90 year old denture patient with no
alveolar ridge, who has a diminished mastication force of 75% forcing that
patient to mash his/her food laterally, distracting the condyles, and
dislodging the dentures? What were the circumstances that
programmed us for the concept of flat plane
occlusion? There were three: one was the
influence of the horizontal function paradigm, but the strongest influence was
some research that was done by Kydd, Regli, Swoope, and Ortman in the 1950s and
60s. [10-13]. These investigators placed strain gauges in dentures and had
patients eat various types of foods with different morphologies of posterior
teeth from 33 degrees to zero degree. The
results: the strain
gauges measured highest with 33 degree teeth
and lowest with the zero degree. Their conclusions were that the increased
strain in the denture with 33 degree teeth would be harmful to the alveolar
bone. Unfortunately, their conclusions lacked understanding. The fact that the
strain gauges registered high with the 33 degree teeth meant that the denture
was working efficiently, directing valuable vertical stimulation to the
alveolar ridge. The zero degree teeth diminished
the alveolar stimulation, dislodging the dentures laterally as the flattened
teeth forced the patient to eat laterally. And finally there is the perception
that our evolutionary blueprint has programmed us for zero degree occlusion and
that all living humans were designed to eat with a flattened dentition.
Neilburger (dentist
and anthropologist) warns that deviation from this
model may cause serious problems for patients and he encourages dentists to aid
in this attrition [14]. He labels this process as normal. It is normal because
it is common, but common isnt necessarily good. It is poor speculation to
declare that we are predestined to have a flattened dentition as evidenced by
the many seniors who maintain naturally sharp teeth. Disordered
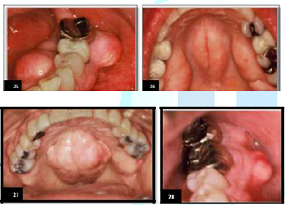
or Perverted Function One reason DCS has been so
successful over the centuries is that it works well within ones subconscious.
Since many patients affected are unaware, the General
Practitioner GP must recognize the visual signs in
order to address the problem. In addition to the obvious signs of a flattened
dentition and hypertrophied muscles of mastication, there are certain
deformations caused by clenching and grinding that many dentists misdiagnose or
dont understand [15]. Nevertheless, these deformations affect the dentition,
bone, and restorative materials. It is to be noted that they are not germane to
each patient affected as there are just too many variables such as the power
and frequency of the compression, the genetic resistance of the alveolar bone,
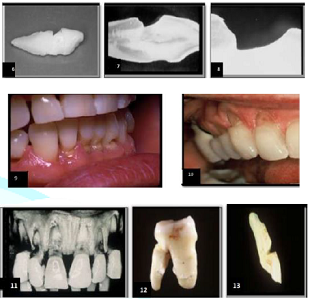
sex, and the biologic strength of the patient. There are four distinct types of
deformations that identify DCS: a non-carious wedge shaped lesion found at the
gingiva (Figure 1), the inverted
cupola, another Non
Carious Lesion (NCL) found at the tips of functional
cusps (Figure 2), exostosis (Figure 3); and deformations of
restorative materials (Figure 4).
Lets look at each. Figure
2: Inverted Cupolas–NCLS Due To
Compression, Static or Cyclic Loading. Figure
4: Luder Lines in Amalgam Due to Stress. Gingival
Ncls A wedge shaped lesion that
usually occurs at the Dentinal Enamel Junction (DEJ) of teeth. It is classified
as a Non-Carious Lesion (NCL). (Figure 5)
What causes it? This unique loss of tooth substance has been the subject of controversy
among dentists for almost one hundred years. W.I.
Ferrier once wrote; ‚their etiology seems to be shrouded in mystery [16]. But
it is not such a mystery if we understand the science of biomechanics, ie; the
study of the mechanical behavior of living materials and structure. What we are
actually seeing are multi-shaped examples of fatigue due to compression and
tension (Figure 6-13). Figure
5: NCLS at the Gingiva Due to Compression and Tension. Figures
6-13: Various Examples of NCLS Due to DCS. Figure
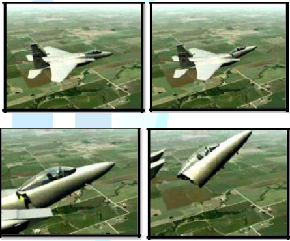
14-17: Structural Failure of Jetfighter Due to
Corrosion Fatigue. Fatigue applies to changes in the
properties of a material due to repeated applications of stress or strain-in
this case, compression failure from DCS. J.E. Gordon, a professor of materials
at Reading University, U.K., describes fatigue as one of the most insidious
causes of loss of strength in a structure [17]. If an object, such as a tennis
ball, rebounds to its original shape after repeated compressions, it is said to
be elastic in nature. However, if an object exhibits residual defects after
repeated compression, it is said to be plastic in nature. Biological
structures, such teeth and bone are termed viscoelastic
and are subject to deformation. Engineers refer to this type of fatigue as
corrosion fatigue. Figures
14-17 show a jet fighter whose Cock pit was
sheared from the body of the plane. The cause is corrosion fatigue which is the
reduction by corrosion, of the ability of the metal to withstand cyclic or
repeated stresses. So, why dont we recognize this? This is an engineering
problem and the mechanisms of engineering are not emphasized in dental school
because engineering is taught in high math-calculus. In dental school, we drop
high math and focus more on chemistry. Since teeth do work, it behooves
us to examine the design aspects of the dentition from an engineering point of
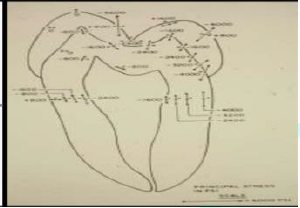
view. In 1975, a team of
engineers at the University of California, Los Angeles, used the finite element
method to study stress generated in a premolar as a result of occlusal forces
[18]. This method is a mathematical technique which is well suited to the
analysis of stress in teeth and dental
restorations because it can closely simulate the
geometrics, loads, and material in homogeneities in the system being studied. The analysis (Figure 18) definitely revealed that the
DEJ was susceptible to cleavage or failure planes. In this example, a failure
plane is apt to occur on the lingual face running through the DEJ well down
into the root-the classic geometry of a gingival notch. A year later, another
team of engineers at Brunel University, Middlesex, England, did a similar study
with supportive results [19]. (Figure 19) Figure
18: Magnitude and direction of principal stresses at selected locations. Figure
19: Axissymmetric finite element model with three marginal
configurations. Again using the finite element
method to demonstrate stress distribution, these engineers concluded the
tensile forces in the gingival area are powerful enough to pull apart the
enamel prisms. They also concluded these high stresses are probably responsible
for the pain often experienced by patients who have received cervically placed
restorations. This was in the pre-bonding era where we would mechanically lock
in our restorations. While these two engineering reports began to reveal
valuable information about the amount of activity in the gingival zone, it was an
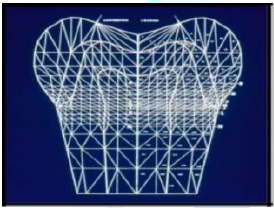
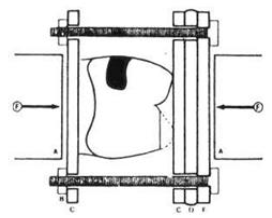
earlier work that demonstrated the unusual flexibility of teeth. In 1968, Dr.
J.A. Hood published an article in the New Zealand dental journal, experimental
studies on tooth deformation [20]. Using the method of photoelasticity
(Figure 20) this researcher placed
teeth in a loading frame and applied pressure. The frozen stress technique
utilized demonstrated an actual shortening of the tooth occlusal-gingivally
with an increase in its bucco-lingual diameter. Figure
20: Compression of Tooth in a Loading Frame
to Demonstrate Flexibility of teeth. Teeth are flexible-a subject
rarely discussed. The
compression failure of an object occurs at its most vulnerable site. Teeth are
most susceptible at the gingival area. If the alveolar bone recedes, the
failure site will also be lowered. Figures
21 & 22 demonstrate defects that appear in tandem as the supporting
bone atrophies thus changing the fulcrum point. Also note in Figure 22 that the only occlusal contact
is on the incline plane, forcing the bicuspid to be flexed toward the lingual
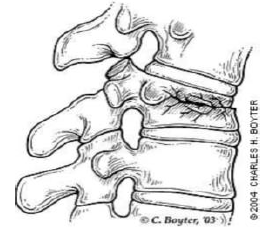
when the patient clenched. Compression fatigue can also occur in the spine (Figure 23). In orthopedics, these sites
of destructive stress are termed compression or wedge
fractures [21]. Sites
of compression fatigue in biological structures are not uncommon and easily
found in professional athletes such as ice
skaters or runners, so it is unfortunate that
many in the dental profession are uncomfortable with their engineering
etiology. Figures
21 and 22: Gingival Fatigue in Tandem. Figure
23: Vertebral Compression or Wedge Fracture. The
Inverted Upola The most common compression NCL
is a perfectly rounded depression sometimes called occlusal dimples, found at
the tips of functional cusps (Figure 24).
Nothing of significance has been written about them except that they are
associated with compression. Although the inverted cupola contrasts
dramatically in geometric design with the wedge shaped NCL, there are two
striking similarities, ie; they are both site specific in that they are found
at sites of high stress on teeth, and they both exhibit a glassy sheen [22].
Kornfeld wrote about this phenomenon in 1932 when he observed that these
defects were hard, smooth, and glasslike in appearance [23]. The author
suggests that this glassy effect is due to the exit of positive ions produced
by the compression of appetite crystals in the dentition and the alveolar bone
[24]. This is the result of the piezoelectric
effect. A piezoelectric substance is one that
produces an electric charge when a mechanical stress is applied causing the
substance to be squeezed or stretched. Conversely, a mechanical deformation is
produced when an electric field is applied. Electricity is composed of both
negative and positive ions. It is suggested that positive ions are being
emitted through these focal points of high stress carrying with them minute
particles of tooth structure. This would not only explain the glassy effect,
but the loss of tooth structure as well. It is not unusual to find these glassy
concavities on the first molars only. The explanation is that these molars
appear first in the transgression from deciduous to secondary dentition and
receive the full force of bruxism that is common during this period. The
compression forces on the six year molars are reduced with the emergence of the
remaining dentition. Figure
24: Compression NCLS-Tips of Functional
Cusps. Note:
It is the stress which results from the various loading forces such as
compression, tension, flexion, and shearing that causes tooth degradation and
its effects on bone and materials. Keep in mind the equation S=F/A, where
stress is concentrated, damage will occur J. Grippo, DDS. Deformation
of Bone-Exostosis Articles on torus
palatinus and torus
mandibularis have appeared since 1814 [25] (Figures 25-28). Although there is no
consensus as to their etiology, many associate their occurance with TMDs and
masticatory hyperfunction [26,27]. Specifically, the negative ions generated
from the compression of appetite crystals are responsible for the aggregates of
new bone growth. This may well explain the metallic taste that people
experience from time to time. Figures
25-28: Examples of exostosis due to
piezzoelectric effect. Deformations
of Restorative Materials Fatigue easily manifests itself in prostheses and restorative materials
such as amalgam and acrylic. In engineering, these
wavy
patterns are called‚ Luder Lines, or molecular slip bands. The explanation for
the patterns is that molecules in the alloy are rearranging themselves under
the influence of compressive strain. One can demonstrate the effect by bending
a metal coat hanger back and forth and examining the stress configuration that
is produced. Figures 29-32
demonstrate Luder Lines in restorative materials. A survey was taken of 100
patients (50 female; 50 male; age range, 17-76) to determine how many exhibited
signs and symptoms of DCS and TMD [28] (Table
1). The deformations in the oral environment
are important diagnostic
tools, but their appearance does not mean
that the patient is currently affected with DCS, as it may have been from a prior
stressful period in their lives. The stomatognathic
system best serves the patient when it functions
vertically and is free from clenching and grinding. If DCS does occur, it is
the obligation of the G.P. to recognize the signs, consult with the patient on
management, ensure that the occlusion (the way the teeth touch each other in
closure) is correct, and provide a guard if necessary. If clenching occurs
during waking hours, it is the responsibility of the patient to monitor
themselves and make a conscious effort to keep their teeth apart (mandible at
rest). If clenching and/or grinding do occur while sleeping, it is the GPs
responsibility to provide a comfortable guard. The main reason for the
occlusion confusion is that we have been accommodating the horizontal component
of DCS instead of trying to prevent it. We have gone from group function, to
cuspid rise, and then to anterior guidance which in my opinion, doesnt make any
sense at all. Anterior guidance, aka mutually protected occlusion, aka mutually
protected articulation according to the Journal of Prosthetic Dentistry is
defined as: An occlusal scheme in which the posterior teeth prevent excessive
contact of the anterior teeth in maximum intercuspation, and the anterior teeth
disengage the posterior teeth in all mandibular
excursions. The general understanding of anterior
guidance is that there is some sort of mutual protection at work here. Nothing
could be further from the truth. Lets examine this concept in detail. Table
1: Signs and Symptoms of DCS and TMD. The
posterior teeth prevent excessive contact of anterior teeth in maximum
intercuspation First of all, why the excessive
contact? We are talking about the vertical form of DCS-clenching. If the
patient is clenching vigorously during waking hours, it is their responsibility
to monitor themselves and control it. If they are clenching with force while
sleeping, a guard will suffice. Is it possible that clenching on the posterior
teeth can prevent excessive contact on the anterior
teeth? Not necessarily. A posterior tooth
will be subject to more stress upon clenching than an anterior tooth simply
because there is more surface contact upon closure, i.e., stress is a result of
pounds per contact unit squared. However, if the occlusal contact upon closure
for both molars and the lingual of the upper
anteriors is equal, so will be the stress. The
anterior teeth will disengage the posterior teeth in all mandibular excursions The idea being that if the
patient is grinding, the posterior
teeth will not wear. This is not logical
thinking and it is harmful. Lets be clear. This is not normal function, this is
parafunction. Im sure there is the exception to the rule, but generally people
do not grind their teeth during waking hours, they clench, and since grinding
in protrusion occurs only while sleeping, a comfortable guard would be the
appropriate protection. This mutual protection theory is flawed in that it does
not address the damage incurred to the anterior teeth during the parafunction.
If this concept were credible, there would be little use for guards. Consequences of the Confusion How
Has the Confusion Affected the Way Dentistry is Currently Being Produced? Restorative
dentistry takes place on two distinct levels; maintaining the status quo and
rehabilitation/reconstruction. Lets look at each. Maintaining the Occlusal Status Quo Benchmark:
The Dentition What
is the current situation? Universally, 99% of restorative
dentistry is done by increments–replacing old or
creating new restorations to maintain the occlusal (The System) status quo. If
the patient has no complaints regarding occlusion (How the teeth touch), the
TMJ, or orofacial pain, the dentist proceeds with the restorative project. If
that project, say a crown or a bridge, opposes a dentition that is naturally
sharp (occlusal surface), the new restoration will correspondingly match its
antagonist. A patient with a flattened dentition will likewise receive a
matching restoration. If there are no interferences in the patients natural
closure or lateral excursions, the new restoration is delivered. What is wrong
with this scenario? What is wrong is that we have the perception that any crown
design is acceptable as long as there are no interferences. This is a
misconception. From an engineering point of view, increased occlusal contact (flattening)
during closure will result in increased stress at the DEJ and widening of the
envelope of function. In addition, the subsequent loss of the intra incline
space will limit anterior-posterior movement of the mandible during postual
changes. Is
there a better way? We have two objectives when
restoring a segment of a patients dentition. The first is to correctly design
the new restoration from an engineering point of view, and the second is to
ensure that it is in harmony with healthy function of the stomatognathic
system. How
is this done? We have a unique problem on our
hands; part engineering and part psychological. This means we have to
accomplish three things; 1. Design
the new restoration to satisfy good engineering principles with the occlusal
contact at the tip of the functional cusp and
touchless incline planes. 2. To
evaluate the stomotognathic system itself for signs of DCS. If the patient is
affected with parafunction the dentist must work with the patient on
management. 3. To
evaluate the remaining dentition to determine whether an equilibration might be
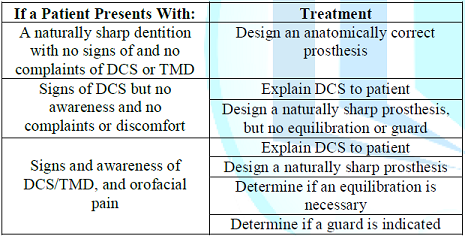
indicated. Table
2: Patient complaints and suggested
treatment. Here
are some general rules Management of DCS begins with the
recognition of the deformations of the dentition, bone, and restorative
materials in the oral environment. This should initiate a dialogue between the
dentist and the patient as to the awareness of the problem since bruxism works
well within the subconscious. So a light discussion, not an accusation is in
order. It should be noted that the observed deformations may have occurred
during a prior time period of stress and the patient may be currently
comfortable. If the patients
occlusion (occlusal contact during closure) is
uncomfortable, it should be determined whether an equilibration is indicated. The
equilibration At the American Equilibration
Societys (AES) 56th meeting in Chicago, there were four speakers;
John Kois, Clayton Chan, Christopher Orr, and Glenn DuPont, each demonstrating
four different methods of equilibration. They all had good results. Which is
the best and simplest method of equilibration for a GP to use when doing piece
meal restorative dentistry? I dont believe it is necessary to use complicated
instrumentation to accomplish an equilibration. I simply apply occlusal
indicator wax on the occlusal surfaces of one arch and have the patient squeeze
once. The areas of displaced wax are analyzed. Where are they? Are they at the
tip of the cusp or on the incline planes? Are they large or small? Ideal
contacts are small and confined to the tips of the cusps and the central
fossae. If the incline planes are touching, I reduce them. If there is heavy
contact in the central fossae I sharpen the opposing functional cusps. I do
check their lateral excursions for interferences, but I warn patients not to go
into these harmful lateral compressions. The teeth are never shortened. The
feeling after an equilibration is one of ‚less. The equilibration reduces the stress
on the teeth and allows greater freedom for the
mandible, however it doesnt mean the patient wont clench if stressed-thats where
the guard comes in. The exception to the rule: the
original morphology of our teeth is superior to that of a flattened dentition.
However, I dont mean to imply that all flat teeth should be equilibrated
(sharpened). I have seen many patients over the years with zero degree
occlusion, and in most cases they are quite comfortable. The damage has been
done. To equilibrate their teeth would be disastrous. However there should be a
general understanding that preserving
the original morphology
of the dentition is superior and more efficient than a flattened dentition. If
patients are actively compressing their teeth while sleeping, then a guard is
mandatory. It is normal for many patients to grind and clench while sleeping.
It just means that their minds are very active or they are dreaming and the
purpose of the guard is not to get them to stop, but to provide an acrylic
spacer to absorb the compressive forces. I once witnessed two poster board displays
at an AES meeting prepared by the graduate students at Northwestern University
Dental School. One was entitled ‚Guards Work‛ and listed all the benefits of
guard therapy. The other poster board was entitled‚ Guards dont work and had a
list of problems that could occur by wearing them. So, whats the point? The
point is that you have to find the right guard for the right patient. I
personally endorse the smaller anterior hard guards as they
reduce the compression force by 75%, but others recommend the larger guard
covering the molars. They point out that their purpose is to support the TMJ.
To my way of thinking it only adds more stress to the TMJ. So here is another
contributing factor to the confusion that needs debate. Note:
Soft guards although comfortable, may encourage clenching and guards should
only be worn while sleeping. Excessive use of a guard during waking hours can
cause micro movement of the teeth. A small percentage of dentists
limit their practices to patients who are severely compromised with problems
relating to occlusion (Stomatognathic System). There are many post graduate
study groups that are dedicated to understanding and solving these problems,
the most noted being the Las Vegas Institute (LVI), The Dawson Group, and the
Pankey Institute. While there is some professional competition between these
groups as to which methodology is superior, they all are very successful,
depending of course, on the skill and experience
of the dentist. The percentage of dentists dedicated to rehabilitation is
estimated at less than 1%. Benchmark:
Muscles of Mastication Benchmark:
Position of the Condyles in the Glenoid Fossae While this all sounds credible
and reasonable, the neutral observer has to ask about the fortification of the
stomatognathic system in order to accept heavy forces. What heavy forces? Arent
we talking about the vertical and horizontal forces of DCS? And since these
heavy forces only occur while sleeping-why not just make them a guard? Again,
we are accommodating DCS rather than trying to prevent it. In
my opinion We have made this subject far
more complicated than it has to be. We have so many conflicting ideas and
theories and practical concepts that a majority of GPs are unsure about what
the right approach should be toward restoration. One unfortunate legacy of the
confusion is that we really dont agree as to the best design of teeth. It is
important that teeth retain their original morphology in order to work
harmoniously so as to not distract the mandible from normal function. Regrettably,
this third, equally important benchmark has been largely ignored. In fact, the
role of the dentition in the function and dysfunction of the system has been
obfuscated to the point that many believe there is no relationship at all.
Ramfjord and Ash reported in 1995; ‚a trend of thinking has developed that
virtually denies any relationship between occlusal (the way teeth touch in
closure) factors and disorders of the masticatory system [29]. Unfortunately,
this attitude is prevalent today. The question is how it could not? Preserving the human dentition in
its natural state is critical to maintaining the health and efficiency
of the system. The prevention of fatigue failure by good design is critical.
Some think design means how it looks, but its really how it works. Maintaining
the original design of the dentition will enable you to produce superior
dentistry. We must examine the morphology of teeth
with a fresh point of view. Vertical function with a naturally sharp dentition
is healthy and efficient. The idea that a flattened occlusal surface is
acceptable is outdated dogma. Sharp teeth are superior.
It is time to look beyond the horizon of antiquated views. What
can we do to clarify the confusion? An important step would be to
stop using the word occlusion in such a broad sense. Being more specific will
simplifies the thought or question. For instance, lets look at two questions
that have plagued us for the past 80 years. What
is an ideal occlusion? Turp et al. discuss the quest for
the ideal occlusion [30]. They explain that an ideal occlusion is rarely found
in real life, that the idea is open to personal interpretation, and that it is
presumptuous to state natures intention for
idealism. I totally disagree. We dont need a clairvoyant to tell us what ideal
is, we just need a bioengineer with some knowledge of physiology. We also need
to be specific about what is meant by the question. If we are concerned about
the stomatognathic
system, an ideal system, no matter class I, II, or III, would be one that
is free from parafunction. The teeth in this parafunctionally free system, no
matter crooked or straight, are naturally sharp, fit loosely with their
antagonists, and have the occlusal contact confined to the tip of the cusp upon
closure. What
is the relationship between occlusion and TMJD? Again, the different
interpretations of the word occlusion make this question difficult to answer.
Lets rephrase the question to: what is the relationship between the
stomatognathic system and TMJD? It is recognized that problems of the TMJ can
be the result of trauma, developmental deformities, or a disease process, but
in my opinion, the vast majority of TMJ problems are the result of repetitive
motion trauma from DCS. In my 40+ years of clinical practice, I have yet to
witness a single case
of TMD that did not have at least one or more signs of parafunction. So a
better question would be; what does parafunction have to do with problems with
the TMJ and then determine whether the occlusal contacts are a contributing
factor. A
call for consensus Every five years, the Japanese
sponsor an international consensus meeting on implantology. Respected
authorities are invited to express their views on important issues and a panel
of judges determines a consensus for each issue for that point in time. Isnt it
about time we had one on occlusion? Until there is a consensus, it is suggested
that general practitioners
follow a simple theme of keeping teeth sharp and keeping them apart. 1.
Christensen
GJ. Personal Correspondence. 11 06, 2008. 2.
Dorland
W. Dorlands Pocket Medical Dictionary 1st Edn (1898) WB Saunders,
Philadelphia. 3.
Dorlands
Pocket Medical Dictionary 20th Edn (1959) WB Saunders, Philadelphia 4.
Jankelson
B, Hoffman GM and Hendron, JA. Physiology of the Stomatognathic System (1953) J
Am Dent Assoc 1953 46: 375. https://doi.org/10.14219/jada.archive.1953.0070 5.
Rugh
JD and Smith BR. A testbook of occlusion (1988) Quintessence Publishing Co,
Chicago 143. 6.
Jablonski
S. Illustrated dictionary of dentistry (1982) WB Saunders, Philadelphia. 7.
Okeson
JP. Management of temporomandibular disorders and occlusion (1993) CV Mosby,
USA 51. 8.
Okeson
JP. Management of temporomandibular disorders and occlusion 3rd Edn
(1993) CV Mosby, USA 125. 9.
McCoy
G. The truth about occlusion (2007) Presented at Yankee Dental Congress San
Francisco. 10.
Ortman
HR. Essentials of complete denture prosthodontics, 2nd Edn Winkler
IN (ed) (1988) PSG Pub. Co, Mosby, USA, 464. 11.
Kydd
WL. Complete Denture Base Deformation with Varied Occlusal Tooth Form (1956) J
Prosthet Dent 6: 714-718. https://doi.org/10.1016/0022-3913(56)90018-X 12.
Regli
CP and Kydd WL. A preliminary study of the lateral deformation of metal base
dentures in relation to plastic base dentures (1953) J Prosthet Dent 3:
326-330. https://doi.org/10.1016/0022-3913(53)90007-9 13.
Swoope
CC and Kydd WL. The effect of cusp form and occlusal surface area on denture
base deformations (1966) J Prosthet Dent 16: 34-43. https://doi.org/10.1016/0022-3913(66)90110-7 14.
Neilburger
E. Flat plane occlusion in the developement of man (1977) J Prosthet Dent 38:
459-469. https://doi.org/10.1016/0022-3913(77)90101-9 15.
McCoy
G. On the Longevity of Teeth (1983) J Oral Implan 2: 248-267. 16.
Ferrier
WI. Clinical observations on erosions and their restorations (1931) J
California State Dent Assoc 20: 1150-1163. https://doi.org/10.14219/jada.archive.1933.0206 17.
Gordon
JE. Structures or Why Things Dont Fall Down (1978) Da Capo Press, USA 333-334. 18.
Selna
LG, Shillingburg HT and Kerr PA. Finite element analysis of dental
structures-axisymmetric and plane stress idealization (1975) J Biomed Matter 9:
237-252. https://doi.org/10.1002/jbm.820090212 19.
Yettram
AL, Wright KWJ and Pickard HM. Finite element stress analysis of the crowns of
normal and restored teeth (1976) J Dent Re 55. 20.
Hood,
JAA. Experimental Studies on Tooth Deformation in Class Five Restorations
(1972) New Zealand Dent J 116-131. 21.
Old
JL and Calvert M. Vertebral compression fractures in the elderly (2004) Am
Family Physician 69: 111-116. 22.
McCoy
G. Examining the Role of Occlusion in the Function and Dysfunction of the Human
Masticatory System (1997) Nippon Dent Rev 659: 163-183. 23.
Kornfeld
B. Preliminary report of clinical observation of cervical erosions (1932) Dent
Items Interest 54: 905-909. 24.
McCoy,
G. Dental Compression Syndrome and TMD, Examining the Relationship (2007) Dent
Today 26: 118-123. Gene
McCoy, San Francisco, California, 94123, USA, E-mail: genemccoydds@sbcglobal.net McCoy
G. Occlusion confusion (2019) Dental Res Manag 3: 16-23Occlusion Confusion
Gene McCoy
Full-Text
Introduction
Occlusion
Confusion
Definition
How many times have you heard of
a restorative failure being blamed on the occlusion? What exactly does that
mean? The question is ambiguous because the word occlusion has three different
interpretations. The original definition was the act or process of occluding
from the Latin, occludere, which means to shut up or close up [2]. Dental
occlusion therefore would be defined as the
relation of the teeth when the jaws are closed nothing more. This was 50 years
ago.
Without a doubt, the biggest
source of confusion comes from the fact that there are two entirely different
viewpoints as to how the stomatognathic system should function.Discussion
The
Morphology of Teeth
Dental
Compression Syndrome
The
Common Denominator for the Sources of Confusion
McCollum and Stuart once talked
about a subtle pathology of function between the opposing teeth and movements
of the mandible. They declared that the lack of understanding regarding this
pathology has kept dentistry from the opportunity to render substantial health
services to our patients. That subtle pathology is Dental
Compression Syndrome (DCS), aka Parafunction, aka
Bruxism. DCS is defined as a total parafunctional daily or nightly activity
that includes grinding, gnashing, or clenching of ones teeth. Capable of forces
in excess of 500 pounds per square inch, DCS can inflict compressive, tensil,
shearing, and flexural forces on the dentition while simultaneously imposing
unwanted force to the alveolar
bone and the TMJ. Our goals in restorative
dentistry are twofold; besides successfully completing the current project,
whether it is a crown, alloy restoration, or denture, it is also our obligation
to keep the patients stomatognathic system healthy and comfortable until the
next restorative project - the biggest threat to that goal is DCS.Signs
of Dysfunction





Conclusion


Epidemiology
Management
of Bruxism

Rehabilitation/Reconstruction
The
Neuromuscular Concept
Using Transcutaneous Electric
Nerve Stimulation (TENS), the goal of neuromuscular rehabilitation is to first
establish a physiologic terminal contact position, i.e.; the myocentric bite.
The incline planes of the teeth are then refined to ensure physiologic
mandibular function. Stabilization of the masticatory system is
achieved by using a removable anatomical orthotic appliance in which cuspid
rise is incorporated.The
Gnathological Approach
The goal of the gnathologist in
the reconstruction/rehabilitation of the stomatognathic system is to obtain an
optimum orthopedically stable joint position. It is called Centric Relation (CR),
and is defined as the position of the condyles when they are in the
anterior-superior position in the glenoid fossae resting against the posterior
slopes of the articular eminences, with the articular discs properly
interposed. This position is considered to be the most musculoskeletally
stable position of the mandible. It is also the objective of the gnathologist
to have stable holding contacts on all teeth to support the condyles in this
centric relation. This position is termed Centric Occlusion (CO). The ultimate
objective gnathological
approach is to establish long-term occlusal stability. This means, as
Okeson explains, to establish an occlusal condition that can accept heavy
forces with minimal damage and at the same time be functionally efficient.Discussion
References
https://doi.org/10.1177/00220345760550060201 *Corresponding author
Citation
Keywords