Review Article :
Fred Saleh and Ghassan Mouhanna Purpose:
The purpose of this study is to survey the existence of specialized pain
clinics/services in rural Lebanon. It also aims at highlighting the importance
of the existence of such clinics/services rurally. Method:
A review of the literature about pain in Lebanon was conducted using PubMed,
Medline, Google Scholars, and Research Gate. Another search was conducted using
Google Maps to locate any specialized pain clinics in the rural areas. The
Lebanese Society for Pain Medicine was also contacted for information about the
distribution of specialized pain clinics/services in Lebanon. Results: Our results
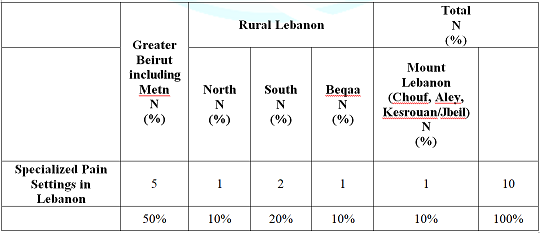
showed that the total number of pain clinics/services in Lebanon is ten. They
are distributed as follows: Five in Greater Beirut including Metn (50%), one in
North Lebanon (10%), two in South Lebanon (20%), one in Beqaa (10%), and one in
Mount Lebanon (Chouf, Aley, Kesrouan/Jbeil) (10%). The majority (90%) of these
services are hospital-based and are governed by the Anesthesia Departments.
Moreover, a comprehensive palliative care approach towards pain management in
terminally-ill cancer and non-cancer patients is still lacking nationwide. Among
such proper health services comes the importance of the existence of
specialized pain clinics in the rural settings. This is based on the fact that
the majority of the rural populations are farmers or technicians, jobs that are
often physically demanding and have high risks of strenuous physical injuries,
let alone exposure to hazardous chemicals. Adding to such risks is the
continuous mental pre-occupation by the
idea of financial survival in the rural villages, which make the rural
residents end up seeking help in relation to not only physical
pain but also to psychosomatic one. Pain is a natural phenomenon. It acts
as an alarming sign that something is going wrong inside our body, or could
occur as a consequence of exposure to thermal, chemical, or physical injuries.
Chronic pain is more than simply an unpleasant physical feeling. It brings one
down on an emotional level too. In fact, one of the main reasons behind
depression is chronic pain, which makes the sufferer goes into a vicious cycle,
whereby chronic pain leads to depression and the latter in turn increases the
perception of the pain. The end product is damage to both mental and physical
health. Globally, 8 of the 12 most disabling conditions are related either to
chronic pain or to the psychological
conditions strongly associated with persistent pain [13]. Non-malignant
chronic pain is one of the most common reasons for primary care visits in
urban cities, let alone in rural areas. However, rural areas do also have
health care disparities, which add to the problem itself. Such disparities have
been documented in relation to culture, beliefs, access to health care,
socioeconomic status, gender, and race. They even have influenced pain
management, since rurality as a social determinant of health has influenced
opioid prescribing [14]. In
a small country like Lebanon, where more than half of the population lives
outside the capital city Beirut, the availability of and
accessibility to specialized pain clinics in rural areas remain a major health
concern. According to the 2017 statistics, the population in Lebanon reached
6,229,794 [15]. This includes around 1.5 million Syrian refugees, and another
half-a-million Palestinian refugees. Rural
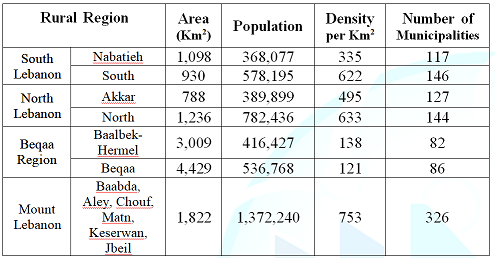
Lebanon is made of four main geographic regions, namely South Lebanon,
North Lebanon, Bekaa, and Mount Lebanon (Table
1). We aimed in this study at surveying the existence of specialized pain
clinics/services in rural Lebanon, and at reflecting on the importance of the
availability of such clinics/services rurally. Table
1: Distribution of Rural regions in Lebanon, and their
Demographics. Materials and
Methods PubMed,
Medline, Google Scholars, and Research Gate were the four search engines used.
We conducted separate searches using a combination of any of the following MeSH
terms “pain, pain clinic, pain intervention, palliative care, migraine,
headache, low back pain, neck pain, shoulder pain, fibromyalgia,
musculoskeletal pain, psychosomatic pain, osteoporotic pain, neuropathic
pain, non-neoplastic pain, neoplastic pain, cancer pain, pediatric pain,
elderly pain”, and “Lebanon”. We searched for such MESH terms in the title
and/or abstracts of the published articles. We then filtered the articles based
on those pertaining to human studies and published in English. No time-frame
was used to filter out old versus new publications. Google Maps was used as a
GIS engine to locate any specialized pain clinic in the rural areas. The
Lebanese Society for Pain Medicine was finally contacted to confirm the results
obtained by Google Maps about the distribution of specialized pain
clinics/services in Lebanon. Our
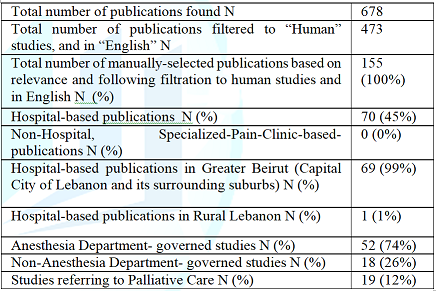
literature search revealed 678 publications that included one or more of the
MeSH terms described in the Materials and Methods section (Table 2). These publications were then filtered to human studies
and in English, followed by manual selection based on relevance of the selected
publications there were 70 hospital-based pain studies (45%), as compared to
none in non-hospital-based specialized-pain clinics (0%). The majority (99%) of
these 70 publications were conducted in Greater Beirut (Beirut City and the
surrounding suburbs), as compared to one study (1%) conducted in Rural Lebanon.
The Anesthesia specialty governed 74% of these studies, as compared to 26%
conducted under other medical or surgical departments. There were 19
publications (12%) referring to palliative care.Our
results also showed that there are currently ten specialized pain settings in
Lebanon. Greater Beirut (Capital City and surrounding suburbs, including Metn)
hosts 50% of these settings, while the remaining ones are distributed in Rural
Lebanon as follows: 1% in North Lebanon, 2% in South Lebanon, 1% in Beqaa, and
1% in Mount Lebanon (Chouf, Aley, Kesrouan/Jbeil) (Table 3). Note: Search engines used PubMed,
Medline, Google Scholars, and Research Gate. Table 2: Publications
about pain in Lebanon. Table
3: Distribution of Specialized Pain
Settings in Lebanon.. Discussion There
were a few striking and surprising features observed in this study. First,
specialized pain clinics or polyclinics are still lacking in Lebanon.
Second, pain management is still hospital-based, and is in the capital city and
its suburbs, leaving rural Lebanon underserved. Third, the majority of pain
management is still conducted through the Anesthesia
Department. Fourth, complementary, alternative and integrative medicine,
including palliative care, still has a long way to go in Lebanon. Fifth,
opioids analgesia for terminally ill cancer and non-cancer patients has not yet
been addressed efficiently by both the public health and legislation
authorities in the capital city Beirut, and the situation is even worse in
rural areas of Lebanon.
Lebanon is a small low-income country where a significant proportion of the
population reside outside the capital city, namely in the North, South, Beqaa,
and the mountain. Despite the continuous help and attempts of the international
community to develop such rural areas of Lebanon, proper and structurally
functional health care systems and services are still lacking. This becomes
more evident when referring to pain management, be it for inpatients or
outpatients. Pain in low- and
middle-income countries, and in rural areas Pain
is often classified as mild, moderate, severe, dull, sharp, localized, diffuse,
sudden, chronic, or as a combination of two or more. Regardless to which of
these categories it belongs, it remains an unpleasant sensation that affects
the rich and the poor, the educated and uneducated, the peasant and the senior
official, the baby, infant, adolescent, toddler, teenager, adult, and elderly.
It is a universal phenomenon regardless of the human race, religion, or
location on planet earth. However, what is different about pain in various
countries is how the health care system is set to alleviate such human
suffering, especially in rural underprivileged communities. In a study
conducted by Jackson and colleagues, the authors investigated the psychosocial
and demographic links with chronic pain solely from Low and Middle-Income
Countries (LMICs), and compared them with current data worldwide [13].
Correlation with rural/urban location, gender, age, education level, insomnia,
depression, anxiety, posttraumatic
stress, disability, income, and additional sites of pain was studied for
each type of chronic pain without clear etiology. Pain was reported in
association with disability in 50 publications, female gender in 40
publications, older age in 34 publications, depression in 36 publications,
anxiety in 19 publications, and multiple somatic complaints in 13 publications.
Females, old patients, and labors in low-education and low-income subgroups
were more likely to have pain in multiple sites, disabilities, and mood
disorders. The authors concluded that recognition
and management of pain are especially crucial in resource-poor geographic
locations like rural areas [13].
Recognition and management of pain in rural areas has also been addressed by a
recent study conducted by Katzman and colleagues through the ECHO Pain project
[16,17]. It is a creative telementoring program for health professionals, which
was created in 2009 at the University of New Mexico Health Sciences Center to
fill considerable gaps in pain management expertise in rural areas. Substantive
proceeding with instruction for clinicians who practice in provincial and
underserved networks assembles week after week by methods for telehealth
innovation. Demonstrations, case-based learning, and didactics are incorporated
into the inter-professional program to improve pain management in the primary
care setting. The project has proven to be a successful continuing professional
development program. The telementoring model seems to compensate for the large
knowledge gap in pain education seen in primary care and other settings.
Expertise is conveyed by implementing effective, work-based and evidence-based
education for diverse health professionals [16].
Living in rural areas, especially in poor countries, is often associated with
low income, stress, work-related injuries, and boredom, to name a few, leading
to psychological
distress, severity of medical illness and dysfunction in conjunction with
psychosomatic pain [18]. Thurston-Hicks and colleagues studied functional
impairment accompanying severity of medical illness and psychological distress
in rural primary care inhabitants, and investigated how such impairment
speckled with chronic medical illness and psychological distress. The authors
reported that the functional impairment was explicated more by psychological
distress than by severity of medical illness. They concluded that decreasing
the burden of psychological distress among primary care patients may improve
functioning [19]. Other studies investigated work-related injuries in rural
areas resulting in pain that is associated with musculoskeletal disorders
(MSDs) [6]. Antonopoulos and co-workers reported that MSDs were common in
patients attending the rural primary care centers in rural Greece, and were
associated with a poor quality of life and mental distress that affected their
consultation behavior [20]. The authors also reported that fewer patients seek
care than those who report symptoms [10]. Dunstan & Covic suggested that
independent, rural or community-based practitioners, working collaboratively
using an integrated treatment program, can yield optimistic results for pain-disabled
injured workers, and attain results similar to those conveyed by urban-based
pain clinics [21]. There
seems to be a shift in low-resource nations, whereby the third epidemiological
transition is becoming prevalent and is characterized by an increase in the
burden of non-communicable health issues. Headache and related disorders make
up a substantial proportion of such health issues. Population growth involving
youthful demographic, and significant rural-urban migration have been witnessed
in low-resource countries. Youthful demographic is often the natural cohort for
migraine, and socioeconomic mobility and modern lifestyle associated with
physical inactivity and obesity are all contributing to headache. Life
expectancy is rising in some resource-restricted countries. This upsurge the
incidence of secondary headache credited to neurovascular causes. Health care
services are chiefly designed to respond to infectious epidemic, and not to
evolving burden like headache,
especially in low-resource-restricted settings that often suffer from
ill-equipped regimes with malfunctioning health policies. As such, headache
treatment and the know-how are scarce in these countries. Addressing the
increasing burden of headache and related disorders in resource-limited
settings is essential to avoid disability, which in turn decreases the
socioeconomic performance in a young booming populace [22]. Palliative
care and the provision of pain relief medicine are essential components of
health care. Palliative care has been an evolving science, and a rapidly
growing specialty in medicine, nursing, and allied health professions in
first-world countries. Palliative care teams now consist of oncologists,
neurologists (pain specialists), palliative care nurse specialists,
complementary and alternative (integrative) medicine specialist (naturopathic
medicine), clinical pharmacists, clinical psychologists, and sociologists.
Palliative care was first identified as a need for terminally-ill cancer
patients, but has been evolving ever since to address chronic pain and related
comorbidity in non-cancer patients [23,24].
In rural areas, the elements that hinder the provision of palliative care
include inadequate access and readiness of pain medication, and providers link
of palliative care with end-of-life care. Satisfactory pain relief is often not
a priority in a busy health care setting. Guaranteeing patients receive
adequate relief for their pain requires interferences at both the clinical and
policy levels. This includes the continuous supply of needed pain medications,
and the training in palliative care for all providers [24].
Pain and depression are common and treatable symptoms among cancer patients,
but they are frequently undertreated and undetected either due to cost or
inexperience [18]. In a study conducted by the Indiana Cancer Pain and
Depression (INCPAD) trial aiming at exploring the incremental cost
effectiveness of the INCPAD intervention, the authors reported that telecare
management coupled with automated symptom monitoring can improve pain and
depression outcomes in cancer patients, and can be cost effective [25]. In
1998, the American Society of Clinical Oncology (ASCO) surveyed its members to
evaluate the practices, challenges, and attitudes associated with end-of-life
care of cancer patients. Pediatric oncologists conveyed a deficiency in formal
courses in pediatric palliative care, and a need for strong role models in this
area. The lack of a reachable pain service or palliative care team was often
identified as a barrier to good care. Another identified hurdle was the
communication difficulty that exists between parents and oncologists,
especially regarding the shift to end-of-life care and adequate pain control.
Integration of palliative care into the routine care of the seriously ill
children through symptom control and psychosocial support has been put in place
[26]. Another
approach to palliative care that has been evolving as well is complementary and
alternative (integrative) medicine (CAM), which also includes herbal medicine
(naturopathic medicine). Although it is beyond the scope of this manuscript to
highlight the pros and cons of CAM, we limit this section to two important
studies for that matter. Guo and colleagues conducted a systematic review and
meta-analysis on the efficacy of injecting the compound Kushen (CKI) in
relieving cancer-related pain. Sixteen trials were identified with a total of
1564 patients. The total pain relief rate of CKI plus chemotherapy was better
than chemotherapy alone, except for colorectal cancer. The treatment groups
achieved a reduction in the incidences of leukopenia, as well as hepatic,
gastrointestinal, and renal functional lesions [27]. In another study conducted
by Denneson and co-workers, the authors reported on prior use and willingness
to try CAM among 401 veterans experiencing chronic non-cancer pain, and
explored the differences between CAM users and nonusers. Participants, who were
recruited in a randomized controlled trial of a collaborative intervention for
chronic pain from five Department of Veterans Affairs (VA) primary care
clinics, self-reported prior use and willingness to try CAM. The authors
detected few differences between veterans who had tried CAM and those who had
not, suggesting that CAM may have broad appeal among veterans with chronic pain
[28]. Opioid
therapy is often controversial and debatable when it comes down to prescription
[29-31]. This is usually due to fear of abuse and addiction. However, the rules
have been more lenient in the past decade, especially when dealing with pain in
terminally-ill cancer patients, but predominantly in the urban and not in the
rural areas. The universal framework to be yet established for using opioids
for chronic pain that is not associated with cancer remains to be seen in both
geographic areas as well. For clinicians, using opioid therapy for chronic non-cancer
pain (CNCP) often results in a conflict between treating their patients pain
and fears of diversion of medication, legal action, or addiction. These
consequent stresses on clinical encounters might in turn unfavorably affect
some elements of clinical care. Buckley and co-workers evaluated a possible
association between Chronic
Opioid Therapy (COT) for CNCP and receipt of various preventive services.
The authors found that patients using COT for CNCP were less likely to receive
some preventive services, such as cancer and lipid profile screening and
smoking cessation counseling [32]. Studies elsewhere have shown that rural
citizens with persistent ache are much more likely to receive an opioid
prescription than non-rural residents. Opioids were taken for pain alleviation
through 76% of the rural citizens, as compared with 52% of the non-rural
residents [33]. Pain Specialists There
are still some debates about the identification of the pain
specialist, including his/her training background, specialty, and
professional and career development in relation to pain management [34]. In a
study conducted by Breuer and colleagues, the authors determined the profiles
of the board-certified pain physician workforce, and the profiles of those
residing near medical pain practices [35]. The 750 respondents were similar to
the entire board-certified group in geographic distribution, age, and primary
specialty. Pain practices were found to be underrepresented in rural areas. The
majority of pain physicians treated chronic pain; 31% worked in an academic
environment; 84% followed patients longitudinally; 29% focused on a single
modality; and 50% had an interdisciplinary practice. Academics were more likely
to be neurologists,
and to have had a pain fellowship. Modality-oriented practitioners were more
likely to be anesthesiologists, and were less likely to provide training to
fellows, follow patients with chronic pain longitudinally, require an opioid
contract, or prescribe controlled substances. The authors reported that
although boarded specialists could benefit from similar curricula and must pass
a certifying examination, their practices varied considerably. They
concluded that data are needed to further elucidate the nature of workforce
disparity, its impact on patient care, and the role of other pain management
clinicians [35]. Other
studies demonstrated that a Clinical
Pathway (CP) enhances pain management in palliative care. However, studies
on CPs in home palliative care, especially in rural areas, are little.
Physicians performing palliative care in rural areas frequently face
characteristic difficulties, and CP could be an effective tool to overcome such
difficulties. Moreover, it could improve adherence to the pain management
guidelines set by WHO [36]. The
specialized pain clinic The emergence of pain specialists, and his/her
integration in the palliative care team as being an essential member who could
function with the team inside and outside the hospital boundaries have led to
the establishment of specialized pain clinics in first world countries. Such
clinics are venues where patients from all age groups irrespective of the
etiology of their pain, be it medical, surgical, orthopedic, traumatic,
oncological, etc., are examined and treated. Visitors of these clinics include
patients with cancer, back pain and radiculopathy, acute herpes zoster and post
herpetic pain, facial neuralgias (trigeminal, occipital, others), painful
peripheral neuropathy (diabetic, drug induced after chemotherapy and
anti-tubercular treatment), headaches including migraine, central pain
syndromes (deafferentation pain) of stroke, phantom limb pain and
post-amputation stump pain, chronic pelvic pain particularly in women,
myofascial and head and neck pain syndromes, fibromyalgias, unusual pain
conditions like HIV, etc. [21,37-50]. We
attempted in this study to shed the light on a universal phenomenon that could
strike anybody, anytime, anywhere, and that is pain. Pain management in Lebanon
still needs proper organization and legislation at various levels. Pain
management protocols should be established for inpatients and outpatients,
and should be unified across the country. Special efforts should be targeted
towards establishing specialized pain polyclinics, and rural areas should be
given upmost priority. Palliative care, be it for cancer or non-cancer patients
with chronic pain, should be a priority, and lessons learned from worldwide
studies should be used to shorten the time frame needed to establish the system
in Greater Beirut, and in the rural areas of Lebanon, namely North, South,
Beqaa, and the Mountain. 1.
Feinberg
T, Jones DL, Lilly C, Umer A and Innes K. The Complementary Health Approaches
for Pain Survey (CHAPS): validity testing and characteristics of a rural
population with pain (2018) PLoS One 13:1-20. https://doi.org/10.1371/journal.pone.0196390 2.
Anderson
FWJ, Naik SI, Feresu SA, Gebrian B, Karki M, et al. Perceptions of pregnancy
complications in Haiti (2008) Int J Gynaecol Obstet 100: 116-123. https://doi.org/10.1016/j.ijgo.2007.08.005 3.
Gorain
A, Barik A, Chowdhury A and Rai RK. Preference in place of delivery among rural
Indian women (2017) PLoS One 12:1-11. https://doi.org/10.1371/journal.pone.0190117 4.
Osaka
R and Nanakorn S. Health care of villagers in northeast Thailand--a health
diary study (1996) Kurume Med J 43: 49-54. https://doi.org/10.2739/kurumemedj.43.49 5.
Dickstein
Y, Neuberger A, Golus M and Schwartz E. Epidemiologic profile of patients seen
in primary care clinics in an urban and a rural setting in Haiti, 2010-11
(2014) Int Health 6:258-262. https://doi.org/10.1093/inthealth/ihu033 6.
Liu
Y, Zhang H, Liang N, Fan W, Jun Li, et al. Prevalence and associated factors of
knee osteoarthritis in a rural Chinese adult population: an epidemiological
survey (2016) BMC Public Health 16:94. https://doi.org/10.1186/s12889-016-2782-x 7.
Davatchi
F. Rheumatology in Iran (2009) Int J Rheum. Dis 12:283-287. https://doi.org/10.1111/j.1756-185X.2009.01425.x 8.
McGraw
IT, Dhanani N, Ray LA, Bentley R.M, Bush R.L, et al. Rapidly evolving outbreak
of a febrile illness in rural haiti: the importance of a field diagnosis of chikungunya
virus in remote locations (2015) Vector borne zoonotic Dis 15:678-682. https://doi.org/10.1089/vbz.2014.1763 9.
Osmun,
WE, Copeland J, Parr J, Boisvert L. Characteristics of chronic pain patients in
a rural teaching practice (2011) Can Fam Phy 57:436-440. 10.
Antonopoulou
M, Antonakis N, Hadjipavlou A and Lionis C. Patterns of pain and consulting
behaviour in patients with musculoskeletal disorders in rural Crete, Greece
(2007) Fam Pract 24:209-216. https://doi.org/10.1093/fampra/cmm012 11.
Lionis
CD, Vardavas CI, Symvoulakis EK, Papadakaki MG, Anastasiou FS, et al. Measuring
the burden of herpes zoster and post herpetic neuralgia within primary care in
rural Crete, Greece (2011) BMC Fam Pract 12:136. https://doi.org/10.1186/1471-2296-12-136 12.
Benesh
LR, Szigeti E, Ferraro FR, Gullicks JN. Tools for assessing chronic pain in
rural elderly women (1997) Home Health Nurse 15:207-211. 13.
Jackson
T, Thomas S, Stabile V, Han X, Shotwell M, et al. Chronic pain without clear
etiology in low- and middle-income countries: a narrative review (2016) Anesth
Analg 122:2028-2039. https://doi.org/10.1213/ANE.0000000000001287 14.
Prunuske
JP, St Hill CA, Hager KD, Lemieux AM, Swanoski MT, et al. Opioid prescribing
patterns for non-malignant chronic pain for rural versus non-rural US adults: a
population-based study using 2010 NAMCS data (2014) BMC Health Serv Res 14:563.
https://doi.org/10.1186/s12913-014-0563-8 15.
World
population prospects: The 2017 revision (2017) Department of economic and social
affairs, Population division volume II: Demographic profiles, UN, New York,
USA. 16.
Katzman
JG. Innovative telementoring for pain management: project ECHO pain. (2014) J
Contin. Educ Health Prof 34:68-75. https://doi.org/10.1002/chp.21210 17.
Shelley
BM, Katzman JG, Comerci GD Jr, Duhigg DJ, Olivas C, et al. ECHO pain
curriculum: balancing mandated continuing education with the needs of rural
health care practitioners (2017) J Contin Educ Health Prof 37:190-194. https://doi.org/10.1097/CEH.0000000000000165 18.
Thommasen
HV, Baggaley E, Thommasen C and Zhang W. Prevalence of depression and
prescriptions for antidepressants, Bella Coola Valley, 2001 (2005) Can J Psych
50:346-352. https://doi.org/10.1177/070674370505000610 19.
Thurston-Hicks
A, Paine S, Hollifield M. Functional impairment associated with psychological
distress and medical severity in rural primary care patients (1998) Psychiatr
Serv 49:951-955. https://doi.org/10.1176/ps.49.7.951 20.
Antonopoulou,
Maria D, Alegakis, Athanasios K, Hadjipavlou, et al. Studying the association
between musculoskeletal disorders, quality of life and mental health. A primary
care pilot study in rural Crete, Greece (2009) BMC musculoskeletal disord 10:143.
https://doi.org/10.1186/1471-2474-10-143 21.
Dunstan
DA and Covic T. Can a rural community-based work-related activity program make
a difference for chronic pain-disabled injured workers? (2007) Aust J Rural
Health 15:166-171. https://doi.org/10.1111/j.1440-1584.2007.00879.x 22.
Woldeamanuel
YW. Headache in Resource-limited settings (2017) Curr pain and headache reports
21:51. https://doi.org/10.1007/s11916-017-0651-7 23.
Denneson
LM, Corson K, Dobscha SK. Complementary and alternative medicine use among
veterans with chronic noncancer pain (2011) J Rehabil Res Dev 48:1119-1128. 24.
Dekker
AM, Amon JJ, le Roux KW, Gaunt CB. What is killing me most: chronic pain and
the need for palliative care in the Eastern Cape, South Africa (2012) J Pain
Palliat Care Pharmacother 26:334-340. https://doi.org/10.3109/15360288.2012.734897 25.
Choi
Yoo SJ, Nyman JA, Cheville AL and Kroenke K. Cost effectiveness of telecare
management for pain and depression in patients with cancer: results from a
randomized trial (2014) Gen Hosp Psychi 36:599-606. https://doi.org/10.1016/j.genhosppsych.2014.07.004 26.
Hilden
JM, Emanuel EJ, Fairclough DL, Link MP, Foley KM, et al. Attitudes and
practices among pediatric oncologists regarding end-of-life care: results of
the 1998 American Society of Clinical Oncology survey (2001) J Clin. Oncol 19:205-212. https://doi.org/10.1200/JCO.2001.19.1.205 27.
Guo
YM, Huang YX, Shen HH, Sang XX, Ma X, et al. Efficacy of compound kushen
injection in relieving cancer-related pain: a systematic review and
meta-analysis (2015) Evid Based Complement Alternat Med 84:7-42. https://doi.org/10.1155/2015/840742 28.
Denneson
LM, Corson K and Dobscha SK. Complementary and alternative medicine use among
veterans with chronic non-cancer pain (2011) J Rehab Res Dev 46:1119-1128. 29.
Click
IA, Basden JA, Bohannon JM, Anderson H and Tudiver F. Opioid prescribing in
rural family practices: a qualitative study (2018) Subst Use Misuse 53:533-540.
https://doi.org/10.1080/10826084.2017.1342659 30.
Buckley
DI, Calvert JF, Lapidus JA and Morris CD. Chronic opioid therapy and preventive
services in rural primary care: an Oregon rural practice-based research network
study (2010) Ann Fam Med 8:237-244. https://dx.doi.org/10.1370%2Fafm.1114 31.
Westanmo
A, Marshall P, Jones E, Burns K, Krebs EE. Opioid dose reduction in a VA health
care system implementation of a primary care population-level initiative (2015)
Pain Med 16:1019-1026. https://doi.org/10.1111/pme.12699 32.
Buckley,
David I, Calvert, James F, Lapidus, et al. Chronic opioid therapy and
preventive services in rural primary care: an Oregon rural practice-based
research network study (2010) Annals fam med 8:237-244. https://dx.doi.org/10.1370%2Fafm.1114 33.
Eaton
LH, Langford D, Meins A, Rue T, Tauben DJ, et al. Use of self-management
interventions for chronic pain management: a comparison between rural and
non-rural residents (2018) Pain Manag Nurs 19:8-13. https://dx.doi.org/10.1016%2Fj.pmn.2017.09.004 34.
Buenaventura
RM, McSweeney TD, Benedetti C, Severyn SA and Gravlee G P. The qualifications
of pain physicians in Ohio (2005) Anesth Analg 100:1746-1752. https://doi.org/10.1213/01.ANE.0000152185.81114.01 35.
Breuer
B, Pappagallo M, Tai JY, Portenoy RK. US board-certified pain physician
practices: uniformity and census data of their locations (2007) J Pain 8:244-250.
https://doi.org/10.1016/j.jpain.2006.08.009 36.
Tateno,
Yuki, Ishikawa and Shizukiyo. Clinical pathways can improve the quality of pain
management in home palliative care in remote locations: retrospective study on
Kozu Island, Japan (1992) Rural and remote health. 37.
ryce
DA, Nelson Glurich JI and Berg RL. Intradiscal electro thermal annuloplasty
therapy: a case series study leading to new considerations (2005) WMJ 104: 39-46. 38.
Chalkiadis
GA. Management of chronic pain in children (2001) Med J Aust 175:476-479. 39.
Pain
relief clinic celebrates 15 years (2014) BDJ 216:608.
https://doi.org/10.1038/sj.bdj.2014.460 40.
Venzke
L, Calvert JF Jr, Gilbertson B. A randomized trial of acupuncture for vasomotor
symptoms in post-menopausal women (2010) Complement. Ther Med.18:59-66. https://doi.org/10.1016/j.ctim.2010.02.002 41.
Gooch
K, Marshall DA, Faris PD, Khong H, Wasylak T, et al., Comparative effectiveness
of alternative clinical pathways for primary hip and knee joint replacement
patients: a pragmatic randomized, controlled trial (2012) Osteoarthr Cartil 20:1086-1094.
https://doi.org/10.1016/j.joca.2012.06.017 42.
Linnemayr
S, Glick P, Kityo C, Mugyeni P and Wagner G. Prospective cohort study of the
impact of antiretroviral therapy on employment outcomes among HIV clients in
Uganda (2013) AIDS Patient Care STDS 27:707-714. Corresponding author:Fred
Saleh, College of Public Health, Phoenicia
University, District of Zahrany, South Lebanon, Lebanon, E-mail: fred.saleh@pu.edu.lb Specialized pain clinic, Rural health, Lebanon.Specialized Rural Pain Clinics:Lessons for a Small Country like Lebanon
Abstract
Background:
People with chronic pain and who live in rural communities often lack access to
pain specialists. They end up relying on primary care providers who may be less
prepared to deal with their conditions.
Full-Text
Introduction
Rural
areas have exceptional health deliberations that eventually consequence in
persistent health discrepancies in outcomes [1-5]. These discrepancies occur
both when comparing urban to rural groups, and when comparing rural subgroups
to each other. Rural communities tend to have unique health
problems, economic concerns, demographic characteristics, resource
shortages, and cultural behaviors that culminate together and thus affect the
health of the residents [1,2,6-12]. Three of the most urgent challenges faced
by rural residents are poverty, education, and access to proper health
services.
Results
Migraine
Palliative
Care
Opioid Therapy
The clinic should be equipped with fluoroscopy for pinpointing accuracy of the
nerve blocks, nonionic radioopaque dyes, steroids like triamcinolone or
depomedrol that have a slow release formulation which sustains the anti-inflammatory
effect for two to three months to ensure that the nerve heals over that time, a
safe technique like radiofrequency for denervation instead of neurolytic agents
like phenol and alcohol which can give rise to neuropathic pain by themselves,
implants like spinal cord stimulators for treating the pain of chronic
backache, refractory angina, failed back surgery etc., intrathecal pumps
tunneled subcutaneously to a pouch in the front of abdomen for other types of
chronic pain and cancer pain, discography to pinpoint the intervertebral disc
to be removed thereby avoiding failure of back surgery, needle procedures like Intra
Discal Electro-thermal annuloplasty (IDET), and nucleoplasty to replace major
invasive back surgery. Conclusion
References
Citation: Saleh F and
Mouhanna G. Specialized rural pain clinics:
lessons for a small country like Lebanon (2019)
Neurophysio and Rehab 1: 6-11 Keywords