Review Article :
Parkinson disease is very common in the world,
ranking second to Alzheimers disease in terms of degenerative neurological
disorders. The disease since 1817 has had so many researchers looking into it,
bringing out symptoms, possible treatment options, causes of the disorder to
mention but a few. There are a number of studies that have looked into the
symptoms of the disorder, especially the non-motor symptoms of the disorder.
This study looks into the motor symptoms associated with the disease. It
brought out the causes, which the study from the literature review conducted
asserted that there is no known cause for it, however, about 60 to 80 percent
of persons with PD, have a degenerating number of dopamine, as such, this can
be postulated to be the cause. The study also affirmed that there is no known
treatment for the symptoms, doctors and medical practitioners would therefore
have to try different forms of treatment till the right one for the patient is
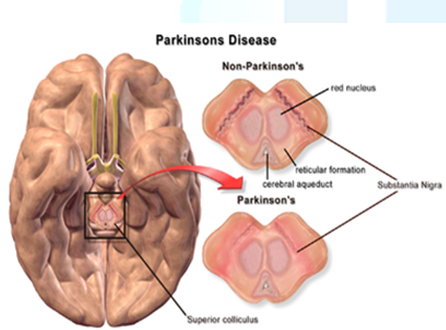
arrived at. Parkinsons disease is the second most common degenerative neurological disorder after Alzheimers disease [1]. The disease has been described by James Parkinson in
1817 as a chronic neurodegenerative disease characterized by the loss of
dopaminergic neurons in the substantia nigra which leads to decreased levels of
dopamine in the striatum and disrupted motor control. Since its description in
1817, there have been a lot of researches being done to understand the
disorder, with some researches being conducted on its prevalence in Sub-Saharan
Africa. This proves that the disease is a worldwide canker which needs much
attention and awareness creation. It is estimated that the disease affects over 1% of the population over the age
of 60, which in the UK equates to over 127,000 individuals (or 500,000
individuals in the USA), while in individuals over the age of 85 this
prevalence reaches 5%, highlighting the impact that advancing age has on the
risk of developing this condition [2-4]. Williams and colleagues [5] reported
in their article on Parkinsons disease in sub-Saharan Africa that the disease
has a prevalence ranging from 7/100,000 in Ethiopia to 67/100,000 in Nigeria,
with the most recent community-based study reporting a mean age at onset of
69.4 years. Since no exact test exists for the diagnosis of PD, the exact
number of people with this disorder cannot be determined, with some being
misdiagnosed because of the diseases similarity to other diseases [6]. Studies have acknowledged that there is a higher chance of PD occurring more in
men than in women [7], with statistics of it occurring in about 50% more men
than women [6]. There is no exact reason for the differences however some
researchers have suggested explanations that, the protective effect of estrogen
in women, the higher rate of minor head trauma, and exposure to occupational
toxins in men, and genetic
susceptibility genes on the sex chromosomes could account for these differences
[7]. Gillies and colleagues [8] are however of the view that the difference is
determined, largely, by biological sex differences in the NSDA system which, in
turn, arise from hormonal, genetic and environmental influences. Over the
years, researches have concluded that the disorder is not inherited, that is it
does not pass down through family line. Though some cases of PD occur in
families, 90% of cases are sporadic, meaning they occur without an, as yet,
identified inherited genetic predisposition [2], simply put, it does not happen
because one of the family member has it.
Recent researches that have been done on PD attempt to look at the causation
factors of PD. The purpose of this paper is to review the large body of
literature on Parkinsons disease, looking at what has been done so far. It is
estimated that the number of people with PD in 2005 was approximately between
4.1million and 4.6 million and that will more than double by 2030 to between
8.7 million and 9.3 million [9]. Towards this regard, the paper aims at
bringing out a comprehensive report on what has been done, with particular
attention to the symptoms of the disease, examining the early stage symptoms
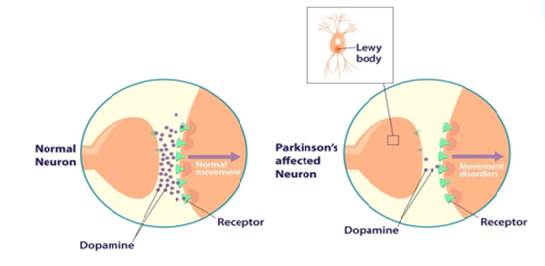
and what people should expect. Genetic predisposing factors in combination with environmental factors are thought
to be responsible for the cellular changes leading to progressive neuronal
degeneration in which mitochondrial dysfunction, oxidative mechanisms and
failure of the protein degradation machinery at the cellular level are probably
involved [14]. The presence of Lewy bodies (cytoplasmic proteinaceous
inclusions) in surviving dopaminergic neurons is the pathological hallmark of
PD [10] (Figures 1 and 2). Figure 2: Dopamine levels in a normal
and a Parkinson’s affected neuron Akinesia
is a term for the loss of ability to move your muscles voluntarily. In
describing this symptom of PD, Kinnier Wilson had this to say it seems as if
the patient does not care to continue the task or put an adequate amount of
effort into a particular movement [20]. Even though a major symptom of PD,
akinesia can also appear as a symptom for other conditions too. According to a
study in the Journal of Neurology, Neurosurgery & Psychiatry, 47 percent of
more than 6,600 people with Parkinsons disease who responded to a questionnaire
reported akinesia or freezing as a symptom. Akinesia is characterized by abnormal stiffness due to increased tone of both
the agonist and antagonist muscles (lead pipe) or cogwheel rigidity due to
superimposed or underlying tumor [21]. Akinesia can also be referred to as
freezing. Some of the symptoms associated with akinesia include difficulty when
a person starts out to walk somewhere, muscle rigidity, usually beginning in
the neck and legs, muscles in the face can also become rigid, similar to a mask
and there is also sudden inability to move the feet properly, especially when
turning or approaching a destination [22]. Usually Parkinson associated
akinesia is brought about as a result of a reduction in dopamine in the brain,
causing a difficulty in the ability to move body parts [22]. Treatments
for Parkinsons disease-related akinesia can be more complicated as no one
treatment can be used or is known to cure this symptom. Doctors will often
prescribe medications that increase the amount of the neurotransmitter dopamine
in the body or the activity it causes. Getting regular exercise can help you
reduce the pain and discomfort that can happen with akinesia and other motor function conditions that may result from PD. It will be advised for a patient
with this symptom to talk to a doctor or a physical therapist about developing
an exercise plan thats comfortable and safe depending on the symptoms and the
progression of akinesia. Exercise has been shown to delay functional decline in
PD. Bradykinesia
has its origination from Greek words slow and movement. The term which
describes slowness in carrying out, rather than initiating, movements was first
used by Dr James Parkinson in 1817. Bradykinesia is one of the early signs of a
movement disorder such as Parkinsons or Parkinsonism. A doctor or neurologist
who observes bradykinesia may well suspect that the person has Parkinsons. The
exact cause of the disorder is unknown [23], however, there are evidence of it
being caused by reduced levels of dopamine in the brain and is often first
noticed by family and friends. Movement is particularly impaired when novel
movements are attempted [24], or when several movements are combined [25,26].
Whereas in akinesia there is the inability to move body parts or a difficulty
in movement, in bradykinesia there is slowness in movement. Theoretically, bradykinesia can be categorized into the verbal-conceptual
models and the mathematical and computational models [23]. The
verbal-conceptual models describe the brain areas, pathways and interactions
thought to lead to parkinsonian bradykinesia whereas the mathematical and
computational models describe the interactions between the various brain areas
involved in movement control and execution that are relevant in parkinsonian
bradykinesia [23]. Bradykinesia cannot be cured; however, the symptoms can be managed somewhat
with medications. The most helpful medications for bradykinesia are those that
increase dopamine levels. Doctors can try various medicines until the right one
for the patient is found. The challenge here will be finding the right
medication for the patient due to the medications becoming less effective over
time. There are therefore other treatment plans that doctors can plan for their
patients. There is the surgical procedure known as deep brain stimulation that
may be used for certain people living with Parkinsons. This treatment involves
surgically placing electrodes into specific locations in your brain. Once the
electrodes are in place, the patient will have electrical impulses sent to
stimulate the brain at the electrode sites. This treatment is normally reserved
for those with severe Parkinson who do not respond well to traditional
medications. The patient can also adopt lifestyle remedies for symptom
management. Usually, whether you are taking medications or not, there are
lifestyle changes and steps a patient with bradykinesia associated with
Parkinson can add at home as part of their treatment plan. However, they should
be sure to talk to their doctor or medical practitioner before adding anything
to the treatment plan. Some of these lifestyle or home treatments may include
eating a healthy diet usually high in fiber, doing physical therapy with
exercises that increase strength, balance, and flexibility like walking and
swimming, and taking the steps needed to help avoid falling [27]. A
tremor is an involuntary quivering movement or shake. It is characterized
clinically by involuntary, rhythmic and alternating movements of one or more
body parts [28]. A consensus statement of the Movement Disorder Society has classified
three tremor syndromes associated with Parkinsons disease [29] to include
resting, postural, and kinetic. Tremor is very common in Parkinsons, affects
about 80% of people with Parkinsons [30]. The tremor that occurs in Parkinsons
disease is different than almost all other tremors because it is a resting
tremor, present primarily at rest [30]. It goes away with movement, but often
returns when the limb (usually a hand or the fingers) is held in one position,
as in holding a spoon or fork to the mouth, which is why those with Parkinsons
are known to spill things. Parkinsons disease tremor may affect almost any part
of the body, but most commonly involves the fingers, followed next most
commonly by the hands, jaw, and feet in that order [30]. The resting tremor is a tremor that occurs during voluntary movements [31].
Resting tremor occurs when the muscle is relaxed, such as when the hands are
resting on the lap. With this, a persons hands, arms, or legs may shake even
when they are at rest [32]. Often, the tremor only affects the hand or fingers.
This type of tremor is also called a pill-rolling tremor because the circular
finger and hand movements resemble rolling of small objects or pills in the
hand [33]. Parkinsonian tremor is caused by damage to structures within the brain
that control movement [32]. This resting tremor, which can occur as an isolated
symptom or be seen in other disorders, is often a precursor to Parkinsons
disease. The symptoms of this tremor can be evidently increased by stress or
emotions. Approximately 70% of PD patients experienced tremor during the course
of the disease [34]. There is no cure for tremor; however, the medication for
the treatment of Parkinsons disease can be used to control this symptom. Rigidity
has been defined by Xia and Rymer [35] as an increased resistance of a joint to
passive movement. The resistance is essentially constant throughout the range
of movement [35]. Rigidity is associated with feeling of stiffness experienced
by the patient, and clinicians may assess rigidity by examining the resistance
of a muscle against passive stretching [36]. One of the major manifestations of
Parkinsons disease is rigidity. The only symptom unequivocally produced by
rigidity is a feeling of stiffness [36]. This term refers to the phenomenon of
increased resistance when stretching a muscle passively. Although some features
of rigidity have been characterized, the detailed physiology is still unknown
[37], it is believed that it is associated with the reduction in dopamine, a neurotransmitter (chemical messenger) that relays the message to particular
areas of the brain to produce smooth, purposeful movement [38]. It has been
estimated that about 90 to 99 percent of people with Parkinsons experience rigidity.
Rigidity is often associated with slowness of movement (bradykinesia). It is
often preceded by aching, stiffness or a feeling of weakness in the muscles
[39]. Everyones experience is different but often rigidity starts in one arm,
spreads to the leg on that side and then to the trunk and other side of the
body. Rigidity will progress faster in some people than in others [39]. Though there is no definite cure for rigidity, a number of treatments could be
applied till the best cure is achieved. Treatment is tailored to the individual
patient and may include medications, surgery (deep brain stimulation), and
complementary or alternative medicine [38]. A physiotherapist can advise on
exercises to maintain or improve both mobility and the range of movement in
muscles and joints. He or she can also suggest strategies to perform daily
activities in a more effective way, for example how to roll in bed or get up
from a chair. An occupational therapist or physiotherapist will be consulted to
advice on devices and aids to help you in your everyday life [39]. Choice of
therapy should be customized to the individual patient with an understanding of
the risks and benefits of each class of medication [40]. The
motor symptoms of PD are the very first symptoms you will notice in a patient
with the disease. Usually, it is the motor symptoms that doctors and other
medical practitioners use as a basis for diagnosing the disease since there is
no definite test. This article looked at literature on the motor symptoms of
the disease, how you can identify them and the steps you can take towards the
treatment. From the researches reviewed it was identified that there is usually
no major known cause for these symptoms, but usually when the motor symptoms of
PD appear, 60 to 80 percent of the neurons that generate dopamine have been
destroyed [6]. It can therefore be concluded that these symptoms are brought
about from the reduction of dopamine. Even in the treatment of these symptoms,
medicines that increase the level of dopamine in the system are recommended. It
was also realized that there was no definite cure for these symptoms just as
the disease itself; however, there are treatments that can help reduce the
problems associated with these symptoms. There has not been much work done on
the reason for the delay in finding a cure for the disease, however, Dr. Soania
Mathur [41] in an article has highlighted some reasons for this, which includes
the brain being too complicated coupled with a complicated disease making it
difficult to find a cure. It can be concluded that drugs that are being
prescribed for Parkinsons can be used to treat these symptoms. There are also
other forms of treatments like medical surgery, exercises and change of
lifestyles that can help with these symptoms. Due to the unknown cure for the
symptoms, doctors would have to try on different treatment plans to arrive at
the best solution for the symptoms. Elbaz
A, Carcaillon L, Kab S and Moisan F. Epidemiology of Parkinsons disease (2016)
Revue neurologique 172:14-26. 2.
De
Lau LM and Breteler MM. Epidemiology of Parkinsons disease (2006) The Lancet
Neurology 5: 525-535. 3.
Nussbaum
RL and Ellis CE. Alzheimers disease and Parkinsons disease (2003) New England J
Med 348: 1356-1364. 4.
Wood-Kaczmar
A, Gandhi S and Wood NW. Understanding the Molecular causes of Parkinsons
disease (2006) Trends in molecular Med 12: 521-528. 5.
Williams
U, Bandmann O and Walker R. Parkinsons Disease in Sub-Saharan Africa: A Review of
Epidemiology, Genetics and Access to Care (2018) J Movement disorders 11: 53. 6.
Parkinsons
Disease. National Institute of Neurological Disorders and Stroke (2014)
National Institutes of Health. 7.
Wirdefeldt
K, Adami HO, Cole P, Trichopoulos D, and Mandel J. Epidemiology and etiology of
Parkinsons disease: a review of the evidence (2011) Eur J Epidemiol 26: 1 8.
Gillies
GE, Pienaar IS, Vohra S, and Qamhawi Z. Sex differences in Parkinsons disease
(2014) Frontiers in neuroendocrinology 35: 370-384. 9.
Dorsey
ER, Constantinescu R, Thompson JP, Biglan KM, Holloway RG, et al. Projected
number of people with Parkinson disease in the most populous nations, 2005
through 2030 (2007) Neurology 68: 6-384. 10.
Albin
RL, Young AB, and Penney JB. The functional anatomy of basal ganglia disorders
(1989) Trends in neurosciences 12: 366-375. 11.
World
Health Organization Neurological disorders: public health challenges (2006) World
Health Organization. 12.
Hamani
C and Lozano AM. Physiology and pathophysiology of Parkinsons disease (2003)
Ann NY Acad Sci 991: 15-21. 13.
Graybiel
AM, Hirsch EC, and Agid Y. The nigrostriatal system in Parkinsons disease
(1990) Advances in neurology 53: 17-29. 14.
Gandhi
S and Wood NW. Molecular pathogenesis of Parkinsons disease (2005) Human molecular
genetics 14: 2749-2755. 15.
Jankovic
J and Tolosa E. Parkinsons disease and movement disorders (2007) Lippincott
Williams & Wilkins, USA. 16.
Kalia
LV, Brotchie JM and Fox SH. Novel nondopaminergic targets for motor features of
Parkinsons disease: review of recent trials (2013) Movement Disorders 28:
131-144. 17.
Xia
R and Mao ZH. Progression of motor symptoms in Parkinsons disease (2012)
Neuroscience bulletin 28: 39-48. 18.
Bohnen
NI, Frey KA, Studenski S, Kotagal V, Koeppe RA et al. Gait speed in Parkinson
disease correlates with cholinergic degeneration (2013) Neurology 81:
1611-1616. 19.
Fox
SH. Non-dopaminergic treatments for motor control in Parkinsons disease (2013) Drugs
73: 1405-1415. 20.
https://www.healthline.com/health/parkinson/akinesia
21.
https://www.slideshare.net/drpsdeb/akinetic-rigid-syndrome 22.
https://www.medicalnewsoday.com/articles/320291.php 23.
Cutsuridis
V. Bradykinesia models of Parkinsons disease (2013) Scholarpedia 8: 30937. 25.
Benecke
R, Rothwell JC, Dick JPR, Day BL, and Marsden CD. Performance of simultaneous
movements in patients with Parkinsons disease (1986) Brain 109: 739-757. 26.
Lazarus
JAC and Stelmach GE. Interlimb coordination in Parkinsons disease (1992)
Movement disorders: official journal of the Movement Disorder Society 7:159-170. 27.
https://www.healthline.com/health/parkinsons/bradykinesia
28.
Abdo
WF, Van De Warrenburg BP, Burn DJ, Quinn NP, and Bloem BR. The clinical
approach to movement disorders (2010) Nature Reviews Neurology 6: 29. 29.
Deuschl
G, Bain P and Brin M. Consensus statement of the movement disorder society on
tremor Ad Hoc Scientific Committee (1998) Movement Disorders 13: 2-23. 30.
https://www.apdaparkin.org/what-is-parkinson/symptoms/tremor
31.
Toth
C, Rajput M and Rajput AH. Anomalies of asymmetry of clinical signs in
parkinsonism (2004) Movement disorders: official journal of the Movement
Disorder Society 19: 151-157. 32.
https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Tremor-Fact-Sheet 33.
http://www.ninds.nih.gov/disorders/tremor/detail_tremor.htm.
34.
Helmich
RC, Aarts E, de Lange FP, Bloem BR, and Toni I. Increased dependence of action
selection on recent motor history in Parkinsons disease (2009) J neuroscience
29: 6105-6113. 35.
Xia
R and Rymer WZ. The role of shortening reaction in mediating rigidity in
Parkinsons disease (2004) Experimental brain research 156: 524-528. 36.
Moustafa
AA, Chakravarthy S, Phillips JR, Gupta A, Keri S, et al. Motor symptoms in
Parkinsons disease: a unified framework (2016) Neuroscience and Biobehavioral
Reviews 68:727-740. 37.
Berardelli
A, Sabra AF and Hallett M. Physiological mechanisms of rigidity in Parkinsons
disease (1983) J Neurology, Neurosurgery and Psychiatry 46: 45-53. 38.
https://parkinsonsdisease.net/symptoms/rigidity
39.
https://www.epda.eu.com/about-parkinsons/symptoms/motor-symptoms/rigidity/
40.
Gazewood
JD, Richards DR and Clebak K. Parkinson disease: an update (2013) Am Fam
Physician 87: 267-73. 41.
http://www.pdf.org/symptoms_primary 42.
https://www.huffingtonpost.ca/soania-mathur/parkinsons-disease-cure_b_9738134.html Agyekum
HA. Motor symptoms of parkinson’s disease -a
review literature (2018)
Neurophysio and Rehab 1: 38-41Motor Symptoms of Parkinson’s Disease – A Review Literature
Hilda Aboagyewaa
Agyekum
Abstract
Full-Text
Introduction
Pathophysiology of PD
Motor Symptoms
Bradykinesia
Conclusion
Connor
NP and Abbs JH. Task-dependent variations in parkinsonian motor impairments
(1991) Brain 114: 321-332.Cocorresponding author:
Hilda Aboagyewaa Agyekum, Department of Social Work, University of Ghana, Ghana, Tel: +233505517635, E-mail: Haagyekum1@gmail.com
Citation:
Keywords
Parkinsons
disease, Alzheimers disease, Dopamine, Substantia nigra, Tremor, Rigidity,
Akinesia and Bradykinesia.